- Thymectomy is a major surgery for MG, often recommended early in diagnosis, especially for those with an enlarged thymus or thymoma.
- This surgery can improve the symptoms of myasthenia gravis, reduce medication dependence, and potentially lead to complete recovery in about 40% of cases.
- Risks include injury, bleeding, lung collapse, infection, and rare myasthenic crises.
- Advances in surgical techniques have significantly lowered complication rates.
Myasthenia gravis (MG) is a rare autoimmune disorder with different treatment options. Most individuals see improvements in their symptoms with oral medications and injectable drugs. However, some may require surgery to combat myasthenia gravis.
Surgery is the standard treatment for a thymus tumor (thymoma). Surgical intervention for MG—thymectomy—may be an option if your symptoms are caused by an enlarged thymus.
In this guide, we will explore the benefits of thymectomy in myasthenia gravis and discuss the potential risks to help you better understand the operation.
Speak to a Specialist
About Copay AssistanceWhy is Thymectomy Recommended?
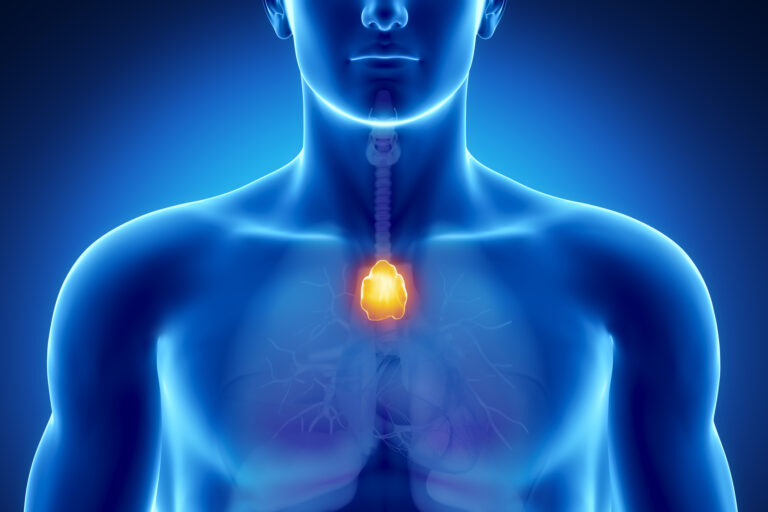
The thymus gland causes the maturation of infection-fighting white blood cells called T cells. This gland plays a pivotal role in the development of myasthenia gravis (MG) [1].
In a minority of people with myasthenia gravis who require surgery, the thymus produces antibodies against acetylcholine receptors in the muscles. As a result, the muscles cannot contract as usual, leading to muscle weakness and fatigue.
The thymus typically starts to shrink after puberty, but not in people with MG. Studies show that about 7 in 10 individuals with MG have enlarged thymus glands. Likewise, nearly 1 in 10 have thymomas [2].
Consequently, surgical removal of the thymus (thymectomy) is a standard treatment. Removing the thymus can help reduce the production of these harmful antibodies and improve overall symptoms of the disease.
Surgery for Myasthenia Gravis: Who Is It For?
Early consideration of surgery may be the best option for certain groups of individuals.
While the decision depends on multiple factors, identifying candidates early can optimize outcomes in those with myasthenia gravis. It can also increase the benefits of thymectomy, such as improved symptom management and reduced medication dependence.
Here are the groups who may benefit from surgery, especially when performed promptly after diagnosis or symptom onset.
Individuals With a Recent Diagnosis
Those who have been recently diagnosed with MG, especially within the first year of symptom development, may experience better long-term outcomes with surgical intervention.
Myasthenia gravis surgery in this group can help:
- Reduce symptom severity
- Modify disease progression
- Lessen reliance on medications
A recent diagnosis often indicates that the immune response is still active and modifiable. This makes thymectomy a strategic option for treating MG.
People With an Enlarged Thymus
An enlarged thymus gland (hyperplasia) or the presence of thymoma (tumor) is a key indicator for considering thymectomy. People with an enlarged gland or a tumor have a higher likelihood of autoimmune activity contributing to their symptoms.
Surgical removal of the thymus in these cases can address the underlying abnormality, thereby reducing disease severity and progression. Those with thymic abnormalities identified via imaging are often considered good candidates for myasthenia gravis surgery.
Young Adults (Typically Below 50)
Younger adults, especially those under 50, tend to have a more active thymus, contributing to disease activity. Early thymectomy in this group may lead to better outcomes, likely because their thymus gland is more reactive and more amenable to removal.
The benefits of thymectomy for myasthenia gravis in this age group include:
- Induced remission
- Reduced medication dependence
- More effective relief of symptoms
- Lowered disease severity over the long term
- Improved overall quality of life
Additionally, younger patients tend to tolerate surgery better, which can contribute to a more favorable prognosis.
Other Groups
Surgery for myasthenia gravis is an ongoing area of research, and more controlled trials are needed to confirm the findings. Recent research suggests that thymectomy can also be considered for MG in older patients, especially if performed early after symptom onset.
A 2019 study highlighted that even in older adults, early surgical intervention, particularly within one year of diagnosis, may lead to improved outcomes [7].
This finding suggests that age alone should not exclude someone from surgical consideration, but timing remains crucial to maximize the benefits of thymectomy in myasthenia gravis patients.
Get Financial Assistance
How is Surgery for Myasthenia Gravis Performed?

Below is an overview of the steps involved in thymectomy.
Step 1: Preparation Before Surgery
Before thymectomy, your medical team will review your health history and perform imaging tests such as CT or MRI scans to assess the tumor or thymic tissue. Pulmonary and cardiac function tests are also conducted to ensure safety.
Step 2: Anesthesia and Positioning
You will receive general anesthesia to ensure you are unconscious and pain-free during the procedure. You’ll be positioned either lying flat or slightly inclined, depending on the surgical approach. The surgeons will also attach monitors to track your vital signs.
Step 3: Surgical Approaches
Myasthenia gravis surgery can be performed in several ways. Your surgical team will determine the best approach based on your condition. Here are the different techniques they may choose from.
Open Surgery (Transsternal)
The surgeon makes a vertical incision along the sternum, then divides the breastbone to access the thymus and carefully removes it.
Minimally Invasive Surgery
- Video-Assisted Thoracoscopic Surgery (VATS): Small incisions are made on the chest wall. A camera, along with surgical instruments, is inserted to dissect and remove thymic tissue.
- Robotic-Assisted Thymectomy: Robotic arms, controlled by the surgeon from a console, are inserted through small chest incisions to perform precise dissection. The benefits of this type of myasthenia gravis thymectomy lie in reduced pain and quicker recovery periods for patients.
Step 4: Thymus Removal
Through one of the above approaches, your surgeon will perform myasthenia gravis surgery and dissect the thymus from surrounding structures, including the mediastinal fat and nearby nerves.
The goal of thymectomy for MG is complete removal of the thymic tissue without injuring vital organs such as the heart, lungs, and nerves.
Step 5: Closure and Recovery
After removing the thymus, the surgeon places chest tubes if necessary to drain fluids or air. The incisions are closed with sutures or staples. You will be monitored closely in recovery for breathing, pain, and other complications.
Step 6: Postoperative Care
Most people stay in the hospital for a few days after myasthenia gravis surgery. Full recovery and a return to normal activities typically take several weeks, depending on the surgical approach.
What are the Benefits of Performing Thymectomy in Myasthenia Gravis Patients?
Thymectomy is an effective treatment that not only improves long-term outcomes but also reduces the need for MG treatment. Even the “International Consensus Guidance for Management of Myasthenia Gravis” recommends it in the following instances [6]:
- During the early stage of the disease
- If your symptoms don’t improve with immunotherapy
- If you cannot tolerate the side effects of immunotherapy
Below, we review the recent literature exploring the potential benefits of myasthenia gravis surgery.
Get Copay Assistance Now
Study 1
According to a 2016 clinical trial, thymectomy plus prednisone is superior to prednisone alone for people with generalized MG. The researchers noted that [3]:
- Those in the thymectomy (with prednisone) group had a lower average quantitative myasthenia gravis score. A lower score indicates less severe symptoms.
- Fewer participants in the thymectomy group required immunosuppression or were hospitalized for flares.
- Participants in the thymectomy group experienced fewer treatment-associated symptoms.
Study 2
In the same year, health experts from the Icahn School of Medicine at Mount Sinai observed similar results in their review. The review concluded that myasthenia gravis surgery was superior to medication-only conservative treatment in improving symptoms [4].
Study 3
In a 2020 investigation, Turkish researchers evaluated the role of thymectomy on recovery. They found that about 40% of individuals who received a thymectomy within 6 months of diagnosis had a complete recovery [5].
Most notably, the benefits of thymectomy in myasthenia gravis included improved recovery, irrespective of the type of MG or duration of the disease.
What are the Complications of Thymectomy for MG?
No surgery is risk-free. Surgery-associated complications are more likely to occur in people with myasthenia gravis, as they can affect breathing. Fortunately, newer surgical and anesthesia techniques have dramatically reduced the risk of such complications.
Death from thymectomy is rare and occurs in fewer than 1% of all cases, even in those with severe MG symptoms. Complications or side effects of thymectomy can include:
- Injury to the heart, blood vessel, or nerve
- Bleeding
- Pneumothorax (collapsed lung)
- Pneumonia (lung infection)
- Fluid or blood accumulation between the lung and the chest wall
- Myasthenic crisis (extremely rare)
What to Expect From Myasthenia Gravis Surgery
Because thymectomy involves the chest, it can be considered a major surgery, typically lasting around 3 hours.
Recovery varies, and symptom improvement does not happen immediately. Most patients see gradual improvements over the first few months, with continued progress over 1 to 2 years.
While thymectomy can reduce symptoms, it’s not a guaranteed cure for MG. Approximately 40% of individuals may experience complete recovery.
You should prepare for a period of healing, follow postoperative care instructions, and attend regular follow-up appointments to see the most benefits of thymectomy in myasthenia gravis symptom improvement.
How AmeriPharma® Specialty Can Support Your Myasthenia Gravis Treatment
Managing myasthenia gravis with or without surgery can be complex. If you’re dealing with this condition and need help, AmeriPharma® Specialty Pharmacy is here to assist you.
Our ACHC-accredited specialty pharmacy offers comprehensive support with hard-to-access medications, full-service coordination, and copay assistance in over 40 U.S. states.
Contact us today to speak to a patient navigator and learn how we can assist you before and after surgery.