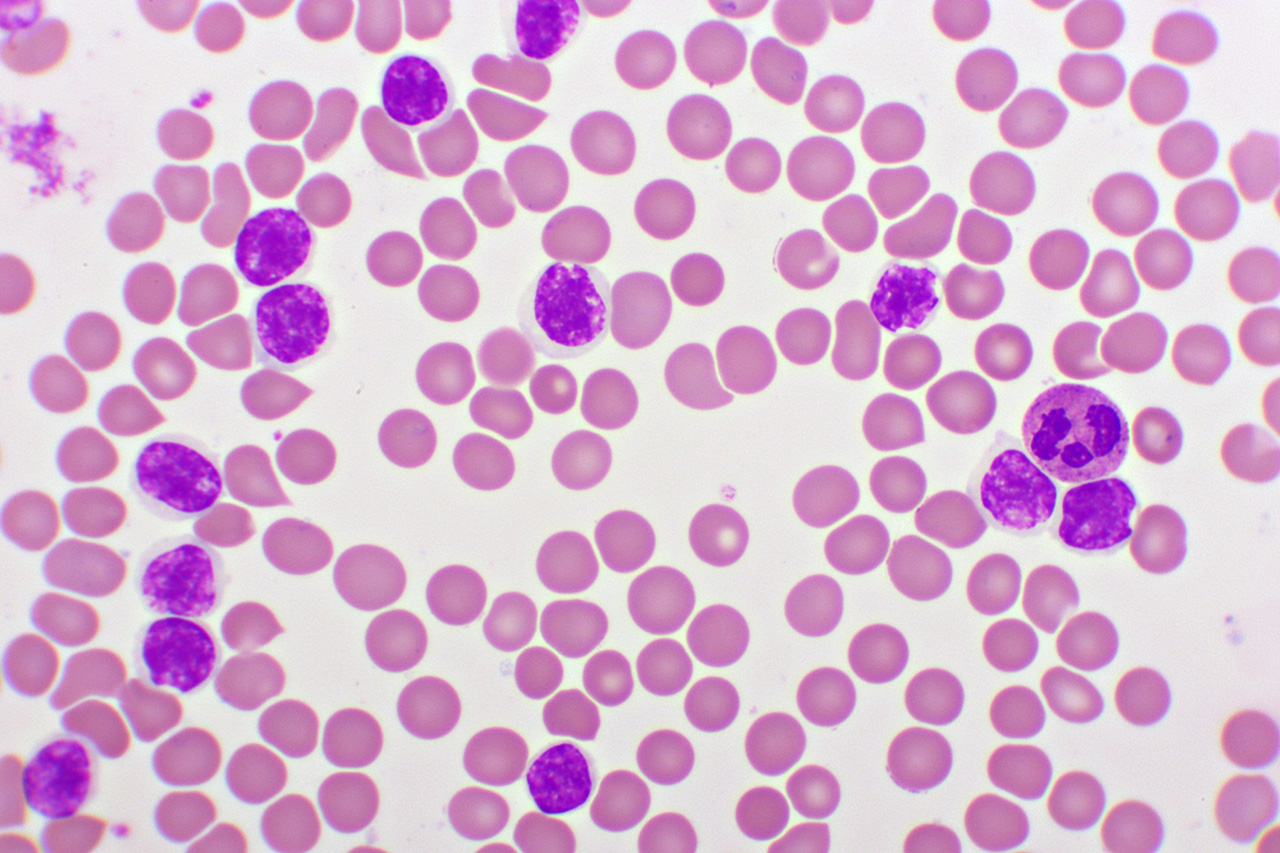
Chronic lymphocytic leukemia (CLL) is a slow-growing cancer that starts in the blood and bone marrow. It mainly affects a type of white blood cell called a B lymphocyte. While CLL is one of the most common leukemias in adults, it’s still relatively rare overall — about 23,000 people in the U.S. are diagnosed each year, which is just 1 – 2% of all cancers. Most people are around age 70 at diagnosis, and it’s extremely rare in children.
Get IVIG Copay Assistance
Speak to a SpecialistYour bone marrow — the soft, spongy tissue inside your bones — is like a factory for blood cells. It houses stem cells that can develop into myeloid stem cells or lymphoid stem cells:
- Myeloid stem cells make red blood cells (carry oxygen), granulocytes and monocytes (fight bacteria and fungi, clean up cell debris), and platelets (help blood clot).
- Lymphoid stem cells make B cells (produce antibodies), T cells (help coordinate the immune response), and natural killer cells (destroy virus-infected and cancerous cells).
In CLL, some B lymphocytes grow, don’t fully mature, and survive abnormally long. These leukemia cells can’t fight infections well, and as they build up, they crowd out healthy blood cells.
CLL Causes and Risk Factors
Doctors don’t know exactly what causes CLL. It’s not strongly linked to radiation, infections, or diet. What we do know is that certain factors raise the risk:
- Age: Risk climbs with age.
- Gender: CLL is slightly more common in males.
- Race: CLL is more common in white people.
- Family history: Having a close relative with CLL increases your chances.
- Chemical exposure: Long-term exposure to certain herbicides or insecticides may play a role.
Treatment Info
Get IVIG Prior AuthorizationSymptoms of CLL
Initially, CLL has no symptoms, but symptoms begin to appear as the disease progresses. The following are the most common symptoms that may occur in CLL patients:
- Enlarged lymph nodes
- Frequent infections
- Unexplained weight loss
- Weakness/feeling tired
- Body pain
- Night sweats
- Anemia
- High temperature
Diagnosis
CLL isn’t something doctors usually screen for. Most people find out they have it when a routine blood test shows a high number of lymphocytes. From there, your doctor will order more tests to confirm the diagnosis and plan treatment.
This often includes:
- Blood tests: A CBC to check cell counts and flow cytometry to see if the lymphocytes are CLL cells.
- Genetic and molecular testing: Looks for TP53 mutations, del(17p), and IGHV status, which help predict how the disease will behave and which treatments will work best.
- Physical exam: Checking for enlarged lymph nodes, liver, or spleen.
- Imaging: CT scans are sometimes used if there’s concern about swollen lymph nodes or organ enlargement.
Biopsy: Bone marrow or lymph node biopsy is only done if blood tests leave questions unanswered.
Life Expectancy in Patients With CLL
Thanks to major advances in treatment, people with CLL are living longer than ever. In the U.S., the overall 5-year survival rate is about 89%, and many live for decades after diagnosis. Your outlook depends on factors like your age, overall health, and specific genetic features of the leukemia. Some people never need treatment, while others may require therapy soon after diagnosis.
Get IVIG Copay Assistance
IVIG Financial AssistanceTreatment Options for CLL
Not everyone with CLL needs treatment right away. If you don’t have symptoms, your doctor may recommend watchful waiting — regular checkups to monitor your health.
When it is time to start treatment, the go-to options today are targeted medicines rather than traditional chemotherapy:
- BTK inhibitors (acalabrutinib, pirtobrutinib, ibrutinib, or zanubrutinib): Pills taken once or twice daily
- BCL-2 inhibitors (venetoclax): pills typically taken once daily
- PI3K inhibitors (Idelalisib, duvelisib): pills taken twice daily,
Your doctor will help decide which is best for you based on genetic tests, other health issues, and your preference for ongoing or time-limited treatment.
Other therapies include:
- Immunotherapy: Monoclonal antibodies like rituximab, obinutuzumab, or ofatumumab, usually given with other targeted therapies..
- Chemotherapy: Now used mainly for a small group of younger, very fit patients with favorable genetics.
- Radiation therapy: Used to shrink swollen nodes or the spleen for symptom relief.
- Stem cell transplant: The only potential cure, but high-risk and used in select cases.
IVIG therapy: For people with low antibody levels and frequent infections — helps prevent infections but doesn’t extend survival.
Consult an IVIG Specialist
The Best IVIG Home Infusion | Get IVIG Treatment AssistanceMost Effective Treatment Plans for CLL
Treatment protocols may change with the stage and severity of cancer and the patient’s general physical health. Treatment options for high-risk patients are different from others.
Some different potential treatment plans are:
- Stem cell transplantation. This is an option if the physical health and fitness of the patient allow it.
- Alemtuzumab, a monoclonal antibody. Monotherapy of this drug proved very effective in more than 60% of the CLL patients. Its efficacy is proved in multiple studies.
- Ibrutinib (Imbruvica). This drug can be used as monotherapy or in combination with rituximab (Rituxan), which may be a better choice to treat lymphoma.
- Venetoclax (Venclexta). Venetoclax can be used as monotherapy or in combination with obinutuzumab (a monoclonal antibody), depending on the condition of the patient and the stage of cancer. Venetoclax is also used in combination with rituximab.
Many complications are associated with chemotherapy treatment and must be managed with an appropriate anticancer drug. Multiple other drugs are used in accordance with the complications of the patient.
REFERENCES:
- American Cancer Society. (2025, March). Cancer facts & figures 2025. Retrieved from https://www.cancer.org/cancer/types/chronic-lymphocytic-leukemia/about/key-statistics.html
- National Cancer Institute. (2025). Cancer stat facts: Chronic lymphocytic leukemia (CLL). Surveillance, Epidemiology, and End Results Program (SEER). Retrieved from https://seer.cancer.gov/statfacts/html/clyl.html
- Chronic lymphocytic leukemia. (2025, July). In Wikipedia. Retrieved from https://en.wikipedia.org/wiki/Chronic_lymphocytic_leukemia
- OncLive. (2024, June 20). Obinutuzumab and liso-cel revisions to CLL/SLL NCCN guidelines mark most notable changes of 2024. Retrieved from https://www.onclive.com/view/obinutuzumab-and-liso-cel-revisions-to-cll-sll-nccn-guidelines-mark-most-notable-changes-of-2024
- OncLive. (2025, January 10). Data continue to refine frontline BTK inhibitor selection in CLL. Retrieved from https://www.onclive.com/view/data-continue-to-refine-frontline-btk-inhibitor-selection-in-cll
- Targeted Oncology. (2025, March 3). Exploring BTK inhibitors for patients with CLL and del(17p) mutations. Retrieved from https://www.targetedonc.com/view/exploring-btk-inhibitors-for-patients-with-cll-and-del-17p-mutations
- Jain, N., et al. (2024). Trends in chronic lymphocytic leukemia survival: SEER data analysis. Journal of Clinical Oncology, 42(15), 1532-1540. https://doi.org/10.1200/JCO.23.02738
- Liu, Y., et al. (2024). Temporal trends in survival for leukemia subtypes in the United States, 1975–2019. PLOS ONE, 19(3), e0314592. https://doi.org/10.1371/journal.pone.0314592













