In the United States, stroke is the fourth leading cause of death, and around 30% to 50% of patients with acute-stage stroke suffer from severe dysphagia. Dysphagia is a condition in which patients experience difficulty in swallowing foods or liquids. This condition often leads to malnutrition and dehydration in stroke patients, with a prevalence rate between 8% and 34%.
Your IV Fluids, Always Available
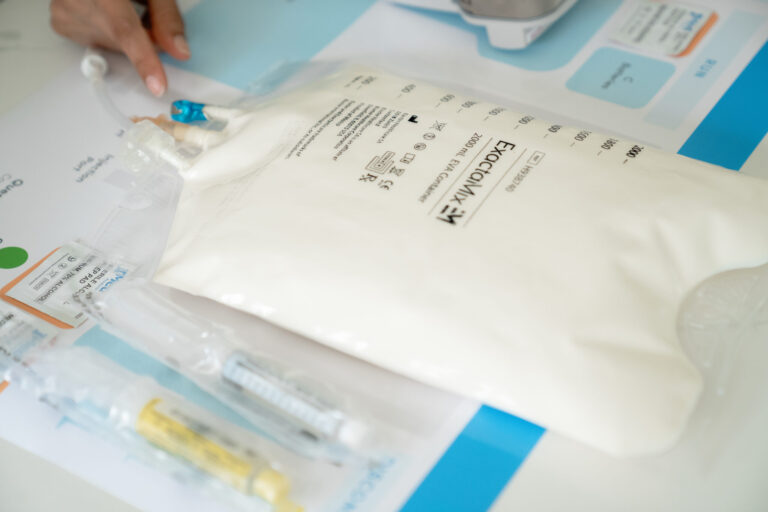
Full inventory, hassle-free accessAlongside medical and rehabilitation treatments, enteral nutrition (EN) is implemented as a first-line nutritional approach for stroke patients to fulfill their nutritional requirements and support overall recovery. However, in some situations, when enteral nutrition does not meet the patient’s nutritional needs, total parenteral nutrition (TPN) is chosen.
In this article, we will provide a comprehensive review of TPN for stroke patients and the circumstances under which TPN is initiated.
What Is a Stroke?
A stroke, also known as a brain attack, is a serious medical condition that occurs when a supply of blood is blocked in a certain region of the brain or when any blood vessel ruptures in the brain. Your brain requires oxygen to function properly, and this oxygen is carried to the brain via blood circulation. However, when the blood circulation is blocked by something, brain cells begin to die due to lack of oxygen, leading to a stroke.
In acute cases, patients may suffer from dysphagia or may end up in a coma after a stroke. To ensure that the patient gets enough nutrition, doctors use enteral nutrition (tube feeding) as a routine measure.
What Is the Role of Total Parenteral Nutrition in Stroke?
Total parenteral nutrition is a nutritional approach in which a balanced mixture of nutrients (such as carbohydrates, proteins, fats, vitamins, minerals, and electrolytes) is delivered directly into the patient’s bloodstream.
The main goal of TPN is to provide proper nutrition to stroke patients who experience difficulties in swallowing food (severe dysphagia), unconsciousness, or other digestive complications.
Though the use of TPN has not been studied in the stroke population, there are a few reports that TPN can be used under certain guidelines for critically ill patients. For example, a study found that providing early nourishment in cases of comatose acute stroke with enteral nutrition did not produce good outcomes. Consequently, they advise that TPN and 20% glucose feeding be started within 48 hours of the beginning of the stroke. Patients can transition to EN after 7–10 days.
Speak to a Specialist About Copay Assistance
When Is TPN Indicated for Stroke Patients?
In general, TPN is not used as a first-line nutritional treatment for stroke due to its cost and complications. Also, no data is available that highlights the effects of TPN in stroke patients. However, under certain situations, TPN can be opted for stroke patients, as follows:
- When enteral nutrition and oral intake are contraindicated or not feasible for stroke patients.
- When a patient has a comatose acute stroke.
- When a patient with an acute phase of severe stroke suffers from diarrhea caused by EN.
- When a well-nourished patient receiving EN for more than 7 days does not meet their nutritional needs. In this case, TPN has to be initiated immediately.
- When sufficient hydration is not provided or not possible through oral intake/enteral nutrition.
If TPN is initiated in the conditions mentioned above, proper measures must be taken to prevent TPN-related complications, mainly hyperglycemia and infection.
In conclusion, the use of TPN has not been studied in stroke patients. However, under certain circumstances, such as when the first-line nutritional approach is not feasible, or the patient’s medical conditions get worse after EN, TPN can be initiated to provide proper nutrition to stroke patients.
REFERENCES:
- Sabbouh, T., & Torbey, M. T. (2018). Malnutrition in stroke patients: risk factors, assessment, and management. Neurocritical Care, 29(3), 374-384. https://doi.org/10.1007/s12028-017-0436-1
- Ojo, O., & Brooke, J. (2016). The Use of Enteral Nutrition in the Management of Stroke. Nutrients, 8(12), 827. https://doi.org/10.3390/nu8120827
- Yamada, S. M. (2015). Too early initiation of enteral nutrition is not nutritionally advantageous for comatose acute stroke patients. Journal of Nippon Medical School, 82(4), 186-192. DOI: 10.4172/2476-2024.1000164
- ARSAVA, E., Aydoğdu, İ., Gungor, L., TOGAY IŞIKAY, C. A. N. A. N., & Yaka, E. (2018). Nutritional approach and treatment in patients with stroke, an expert opinion for Turkey. Turkish Journal of Neurology, 24(3). DOI:10.4274/tnd.92603
- Wirth, R., Smoliner, C., Jäger, M., Warnecke, T., Leischker, A. H., Dziewas, R., & DGEM Steering Committee*. (2013). Guideline clinical nutrition in patients with stroke. Experimental & translational Stroke Medicine, 5, 1-11. https://doi.org/10.1186/2040-7378-5-14