
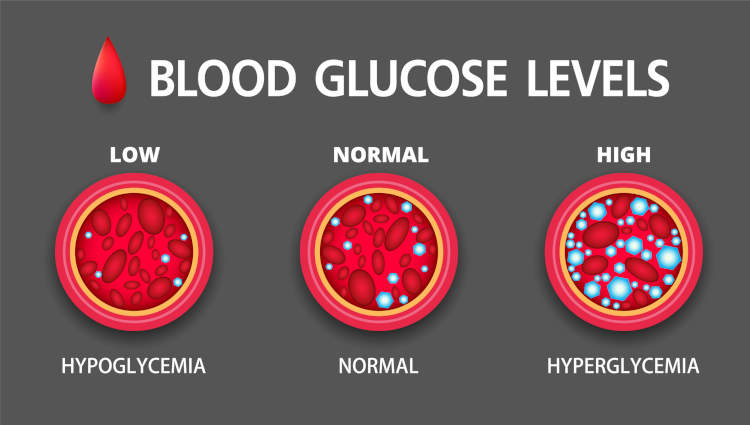
If you or your loved one are receiving total parenteral nutrition (TPN), it is important for you to become aware of the potential risks and complications associated with this therapy. Though TPN has proven to be an effective method for improving the nutritional status of malnourished patients in people who can’t consume food or drink, it can also lead to complications, such as hyperglycemia — a condition characterized by abnormally high blood sugar levels.
Always in Stock
Full inventory of IV fluids, ready for youHyperglycemia is the most common complication in people receiving TPN. It can occur in almost half of hospitalized patients receiving TPN therapy. Moreover, a research study published in Diabetes Care showed that non-critically ill patients who experience hyperglycemia after TPN have a more than fivefold increased risk of mortality (death) during their hospital stay.
In this article, we will explore the relationship between TPN and hyperglycemia, its potential causes, and practical strategies to manage blood sugar levels for patients undergoing TPN.
Understanding TPN and Its Role in Hyperglycemia
TPN is a highly effective method of delivering complete nutrition to patients intravenously. It involves the infusion of a specialized solution containing carbohydrates, proteins, fats, vitamins, and minerals directly into the bloodstream. While TPN is essential for individuals who are unable to eat or absorb nutrients orally, it can lead to the development of hyperglycemia, a condition in which a patient’s blood glucose level is high before or after receiving TPN.
Hyperglycemia during TPN administration increases the risks of acute renal injury, cardiac complication, blood infection (sepsis), and mortality.
Link of TPN with Hyperglycemia
The connection between TPN and hyperglycemia stems from the high glucose content present in TPN solutions. These glucose-rich formulas are necessary to meet the body’s energy requirements, but the excess glucose can overwhelm the body’s ability to regulate blood sugar levels, particularly in individuals with impaired insulin production or sensitivity.
Research studies, randomized trials, and meta-analyses have reported the link between TPN and hyperglycemia among hospitalized patients. For instance, in a recent study involving 88 non-diabetic patients receiving TPN, researchers found that 56% (49 cases) of the patients experienced hyperglycemia. Among these cases, 70% occurred within the first week of TPN administration. In addition to this, some patients even had persistent hyperglycemia for over 4 weeks from the start of TPN.
What are the Potential Causes of Hyperglycemia?
There are several factors that can contribute to the development of hyperglycemia during TPN.
High Glucose Concentration
TPN solutions usually contain higher amounts of glucose (dextrose) than what the body typically encounters. This excess glucose surpasses the body’s capacity to regulate blood glucose levels. Generally, blood glucose levels above 180 mg/dl are considered to be hyperglycemic in the context of TPN. However, the target blood glucose range may vary depending on the specific patient and the healthcare provider’s recommendations.
According to a research report, elevated blood glucose levels above 180 mg/dl pose a higher mortality risk for TPN patients. Similarly, another study showed that patients with blood glucose levels of 137 mg/dl or higher had a 2 to 5 times greater risk of mortality and a 4 to 5.5 times higher incidence of complications than those with blood glucose levels below 114 mg/dl.
Stress
Elevated blood glucose levels could also occur from stress during hospitalization. Factors such as surgery, acute illness, and trauma also raise levels of stress hormones like cortisol and catecholamines as well as inflammatory cytokines. These stress mediators interfere with carbohydrate (glucose) metabolism, which in turn, increases the glucose level in the blood, leading to hyperglycemia.
Ask About TPN Home Infusion
Insulin Resistance
Patients receiving TPN may have pre-existing insulin resistance, which means their cells do not respond effectively to insulin, a hormone that helps your body regulate blood sugar levels. Insulin resistance can make it more challenging to control blood glucose levels during TPN.
Inadequate Insulin Supply
Generally, insulin is responsible for moving glucose from the bloodstream into cells for energy utilization and storing excess glucose in the liver for later use. However, if the body does not produce enough insulin or if there are difficulties with insulin administration, blood sugar levels can rise, causing a hyperglycemic state.
Underlying Medical Conditions
Certain medical conditions, such as diabetes mellitus, sepsis, or pancreatitis, can cause a higher risk of developing hyperglycemia during TPN.
How To Manage or Prevent Hyperglycemia During TPN
Controlling blood sugar levels during TPN is crucial to prevent the complications associated with hyperglycemia. By following the below strategies, you and your healthcare provider can manage hyperglycemia:
- Regular blood glucose monitoring: Frequent monitoring of blood sugar levels helps healthcare providers make necessary adjustments to TPN formulations, insulin doses, and other interventions to maintain optimal blood sugar control. However, if you’re receiving TPN at home, you should ask your provider how often you need to check your blood sugar level.
- Individualized TPN formulation: Healthcare providers tailor TPN solutions to each patient’s specific needs, including adjusting the glucose concentration and other nutrient components to minimize the risk of hyperglycemia.
- Insulin therapy: Insulin therapy can help control blood sugar levels during TPN. Whether given as a subcutaneous injection or intravenously via IV infusion, insulin effectively manages hyperglycemia. The dosage and timing of insulin administration are determined based on blood glucose levels and the individual’s insulin requirements.
For instance, if a patient with diabetes is receiving TPN with 150 grams to 300 grams of carbohydrates per day, adding insulin at a ratio of 1 unit per 11 g of dextrose can be an effective initial step in preventing and reducing hyperglycemia.
- Gradual transition: When transitioning from TPN to enteral nutrition (feeding through the gastrointestinal tract), a gradual approach helps the body adapt to the change, reducing the risk of glucose fluctuations.
Get Financial Assistance for TPN
Conclusion
Hyperglycemia, or high blood glucose level, is one of the most common complications associated with TPN therapy. By understanding the causes and implementing effective management strategies, you and your healthcare provider can maintain optimal blood sugar control and prevent complications associated with hyperglycemia. In addition to this, regular monitoring, individualized TPN formulations, insulin therapy, and gradual transitions from TPN to enteral feeding are some of the key components in achieving successful TPN outcomes while minimizing the risk of hyperglycemia.
REFERENCES:
- Pasquel, F. J., Spiegelman, R., McCauley, M., Smiley, D., Umpierrez, D., Johnson, R., Rhee, M., Gatcliffe, C., Lin, E., Umpierrez, E., Peng, L., & Umpierrez, G. E. (2010). Hyperglycemia During Total Parenteral Nutrition: An important marker of poor outcome and mortality in hospitalized patients. Diabetes Care, 33(4), 739-741. https://doi.org/10.2337/dc09-1748
- Gosmanov, A. R., & Umpierrez, G. E. (2013). Management of Hyperglycemia During Enteral and Parenteral Nutrition Therapy. Current diabetes reports, 13(1), 155. https://doi.org/10.1007/s11892-012-0335-y
- Elizabeth, P., Rogelio Ramón, P., & Félix Alberto, M. (2020). Hyperglycemia associated with parenteral nutrition in noncritical patients. Human Nutrition & Metabolism, 22, 200114. https://doi.org/10.1016/j.hnm.2020.200114
- Lin, L., Lin, H., Lin, H., Lee, P., & Ma, W. (2007). Hyperglycemia Correlates with Outcomes in Patients Receiving Total Parenteral Nutrition. The American Journal of the Medical Sciences, 333(5), 261-265. https://doi.org/10.1097/MAJ.0b013e3180536b26
- Lee, H., Koh, S. O., & Park, M. S. (2011). Higher dextrose delivery via TPN related to the development of hyperglycemia in non-diabetic critically ill patients. Nutrition Research and Practice, 5(5), 450-454. https://doi.org/10.4162/nrp.2011.5.5.450
- Olveira, G., Tapia, M. S., Ocón, J., Cabrejas-Gómez, C., Ballesteros-Pomar, M. D., Vidal-Casariego, A., Arraiza-Irigoyen, C., Olivares, J., Conde-García, M. C., García-Manzanares, Á., Botella-Romero, F., Quílez-Toboso, R. P., Cabrerizo, L., Matía, P., Chicharro, L., Burgos, R., Pujante, P., Ferrer, M., Zugasti, A., . . . Tous, M. C. (2013). Parenteral Nutrition–Associated hyperglycemia in Non–Critically Ill inpatients increases the risk of In-Hospital mortality (Multicenter study). Diabetes Care, 36(5), 1061–1066. https://doi.org/10.2337/dc12-1379
- Ma, J., Gao, M., Pan, R., He, L., Zhao, L., Liu, J., & Liu, H. (2018). Hyperglycemia is associated with cardiac complications in elderly nondiabetic patients receiving total parenteral nutrition. Medicine, 97(6), e9537. https://doi.org/10.1097/md.0000000000009537
- Kumar, P. R., Crotty, P., & Raman, M. (2011). Hyperglycemia in Hospitalized Patients Receiving Parental Nutrition Is Associated with Increased Morbidity and Mortality: A Review. Gastroenterology Research and Practice, 2011, 1–7. https://doi.org/10.1155/2011/760720













