What Is ITP?
Idiopathic Thrombocytopenic Purpura (ITP) is an immune disorder that manifests through abnormal blood clotting. The term “immune thrombocytopenia” is used more commonly to refer to this condition.
ITP is caused by a low platelet count in the blood. Excessive bleeding and bruising can occur as a result of ITP.
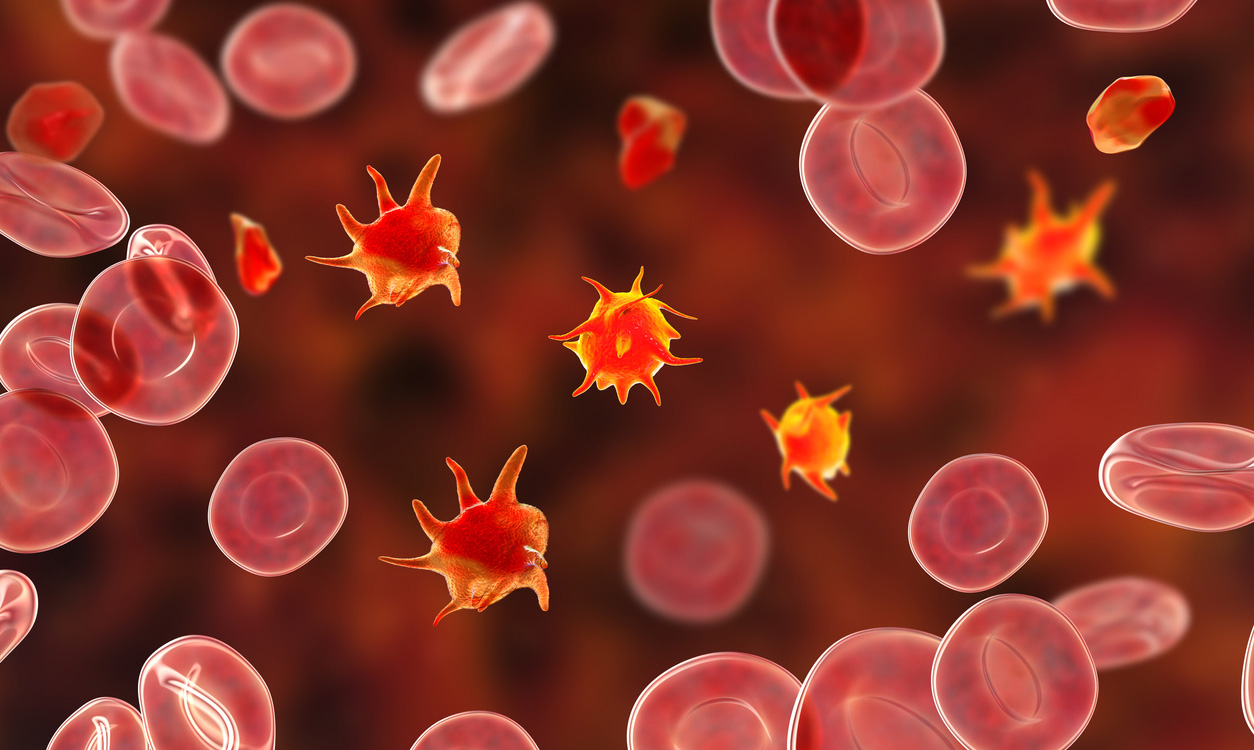
The bone marrow is responsible for the production of platelets. When they clump together, they form a clot, which seals small tears or cuts in the blood vessel and tissue walls, resulting in the cessation of bleeding.
When your blood doesn’t have enough platelets due to idiopathic thrombocytopenic purpura, it clots more slowly. As a result, it is possible to experience internal bleeding as well as bleeding on or beneath the skin.
Get IVIG Copay Assistance
Speak to a SpecialistWhen someone has immune thrombocytopenic purpura (ITP), they develop numerous purple bruises on their skin or mucous membranes inside their mouth. In addition to bruises, petechiae, which are small red or purple dots on the skin, can appear with these bruises. Petechiae is frequently confused with a rash.
ITP is a medical condition that can affect children and adults of any age. According to the data available, the development of idiopathic thrombocytopenic purpura appears to differ between men and women at certain ages. Adult females may be more susceptible to developing ITP.
ITP Types
There are two distinct subtypes of ITP: acute (short-term) and chronic (long-term).
Acute ITP
Acute ITP is a shorter form of immune thrombocytopenic purpura that usually lasts less than six months.
It is the most common type of ITP, and it primarily affects children. It frequently occurs in children after contracting an infection or illness caused by a virus.
Chronic ITP
Chronic ITP is a long-term infection that can last for six months or longer. Generally speaking, it affects adults, but it can also affect adolescents and children.
Even people who have severe forms of chronic idiopathic thrombocytopenic purpura can live for decades. Most people who have chronic ITP can stop treatment at some point and maintain a safe platelet count.
What Is the Cause of Idiopathic Thrombocytopenic Purpura?
The term “idiopathic” refers to a condition with an unknown origin. This term was previously used to describe ITP because the cause was unknown when the disease was first identified.
It is now well established that the immune system plays a significant role in the development of ITP, which has led to the disease’s more recent designation as immune thrombocytopenic purpura.
In adults, infection with HIV, hepatitis, or H. pylori (the type of bacteria that causes stomach ulcers) may trigger this condition. In most children, idiopathic thrombocytopenic purpura follows a viral illness, such as the mumps or the flu.
Can IVIG help?
Free IVIG Treatment Info | Difficulty In Diagnosing?Symptoms of ITP
The following are the most common symptoms of ITP:
- Blood in the stool
- Blood in the urine
- Bruises that occur easily
- Spontaneous nosebleeds
- Prolonged bleeding from cuts
- Abnormally heavy menstruation
- Profuse bleeding during surgery
- Pinpoint-sized petechiae on the lower legs
- Bleeding from the gums (like in dental procedures)
Some individuals with ITP have no symptoms.
What Is the Procedure for Diagnosing Idiopathic Thrombocytopenic Purpura?
Your doctor will perform a comprehensive physical examination and inquire about your medical history and any current medications you are taking.
Your doctor will also order a complete blood count (CBC), among other tests. Recommended follow-ups for idiopathic thrombocytopenic purpura may include a blood test to check for platelet antibodies.
A blood smear will also need to be performed. This test involves placing a small amount of blood on a glass slide. The slide is then observed under a microscope to examine the platelets and other blood cells.
If your doctor determines you have a low platelet count, a bone marrow test may also be recommended. If you have immune thrombocytopenic purpura, the bone marrow in your bones will be normal. If your bone marrow is abnormal, it is almost certain that your low platelet count is the result of a disease other than idiopathic thrombocytopenic purpura.
Available Treatment Options for ITP
It is up to your doctor to determine the best course of treatment for you based on the number of platelets in your blood and the frequency and amount of bleeding you have experienced.
In some cases, medical intervention is not required. Children who develop the acute form of ITP, for example, typically recover without treatment within a few weeks or months.
Adults who have milder cases of ITP may also be able to avoid treatment in some instances. However, your doctor will likely monitor your platelets to ensure you don’t need additional treatments for idiopathic thrombocytopenic purpura in the future.
If your platelet count drops too low, you run the risk of bleeding and will often require treatment.
Consult an IVIG Specialist
The Best IVIG Home Infusion | Get IVIG Treatment AssistanceMedications
If you or your child requires medical attention, your doctor will almost certainly start with medication to alleviate your symptoms. Immune thrombocytopenic purpura is treated with several different medications, which are listed below.
Intravenous Immunoglobulin (IVIG)
The administration of intravenous immunoglobulin may be necessary if your bleeding has reached a critical level or you are scheduled for surgery for idiopathic thrombocytopenic purpura. In these cases, your platelet count needs to be increased as soon as possible.
Immunoglobulin Anti-D
This medication is for people who have Rh-positive blood with functional spleens.
Corticosteroids
Your doctor may prescribe a corticosteroid such as prednisone to increase your platelet count. Once your platelet count is back to a safe level, you can gradually discontinue taking the drug under the direction of your doctor.
Long-term use of corticosteroids is not recommended because they can increase your risk of infections, high blood sugar, and osteoporosis.
Antibiotics
Helicobacter pylori, the bacteria that causes the vast majority of peptic ulcers, has been linked to idiopathic thrombocytopenic purpura in a small number of people.
Some individuals have benefited from antibiotic therapy to eradicate helicobacter pylori, which has been shown to increase platelet counts.
Thrombopoietin Receptor Agonists
Medications such as romiplostim (Nplate) and eltrombopag (Promacta) work by stimulating the production of platelets in the bone marrow, which helps prevent bruising and bleeding in patients with immune thrombocytopenic purpura.
These types of drugs can increase your risk of blood clots.
Get IVIG Copay Assistance
IVIG Financial AssistanceSurgery
Your doctor may recommend spleen removal surgery (splenectomy) if you have severe ITP and your symptoms or platelet count does not improve after taking medication.
The spleen makes antibodies (proteins) that help fight infections. In idiopathic thrombocytopenic purpura, these antibodies destroy platelets by mistake. Therefore, removing the spleen will reduce the destruction of platelets.
Surgery may raise your risk of infections, so your doctor may give you vaccines to help prevent infections before your surgery.
What Is the Emergency Treatment for Idiopathic Thrombocytopenic Purpura?
Some people who have ITP with severe bleeding may require platelet transfusions and hospitalization. Platelet transfusions may also be needed before surgery.
Lifestyle Modifications
Your doctor may recommend that you make the following changes to your lifestyle following idiopathic thrombocytopenic purpura:
- Engage in low-impact activities rather than competitive sports or other high-impact activities since this can help reduce the risk of injury, bruising, and bleeding.
- Consume alcohol in moderation because it has the potential to impair blood coagulation.
- Exercise caution when using over-the-counter medications such as aspirin and ibuprofen since they may impair platelet function.
Treatment of Immune Thrombocytopenic Purpura During Pregnancy
In pregnant women who have ITP, the condition usually will not affect the baby. However, some babies may be born with or develop low platelet counts soon after birth.
The babies’ platelet counts almost always return to normal without any treatment. However, treatment can speed up recovery in babies with very low platelet counts.
Treatment for idiopathic thrombocytopenic purpura during pregnancy depends on a woman’s platelet count. If treatment is needed, the doctor will take a close look at its possible effects on the unborn baby.
Women who have mild cases of ITP can usually go through pregnancy without treatment. Pregnant women who have very low platelet counts or a lot of bleeding are more likely to have heavy bleeding during delivery or afterward.
To prevent heavy bleeding, these women usually receive some form of treatment.
What Is the Outlook for Idiopathic Thrombocytopenic Purpura?
Most people who suffer from immune thrombocytopenic purpura do not have a serious or life-threatening illness.
Children with acute idiopathic thrombocytopenic purpura who do not receive treatment will typically recover within six months or less.
Chronic ITP can last for several years or even decades. Those suffering from severe cases can still expect to live for decades. Many people with ITP can safely manage their condition and avoid long-term complications.
Treatment Info
Get IVIG Prior AuthorizationConclusion
If you or your child develops unexplained bruises or bleeding, you must seek medical attention right away. A wide range of illnesses can cause bleeding and bruising issues, including the flu.
It is possible that the diagnosis will be idiopathic thrombocytopenic purpura and that the prognosis will be favorable. In some cases, treatment is necessary to prevent or manage complications that may arise.
It is crucial to seek medical attention as soon as possible if symptoms return, even if you are currently taking medication for your condition or your condition appears to be improving for some time.
Once the doctor diagnoses your condition, you can receive treatment from AmeriPharma™ Specialty Pharmacy. We offer at-home IVIG infusions to those battling idiopathic thrombocytopenic purpura.
Our specialty pharmacy can even send specialized infusion nurses to your home to administer the treatment and help you troubleshoot any problems. Contact us now to receive specialty care at home with full-service coordination, 24/7/365 support, and copay assistance.
FAQs
Can immune thrombocytopenic purpura be cured?
While there is no cure for ITP, many patients find that their platelet counts improve following treatment. The challenge for many ITP patients is finding a treatment that works for them without unwanted side effects.
Some patients report that changing their diet or lifestyle helps them feel better. The disease can go into remission for a long time, perhaps for the remainder of a person’s life. But idiopathic thrombocytopenic purpura can also recur.
There is currently no way to predict the course of the disease.
What is the cause of idiopathic thrombocytopenic purpura?
It is not known what causes some people to develop ITP, but it is known that ITP causes the body’s immune system to destroy healthy platelets, which can lead to easy or excessive bruising or bleeding.
Some cases appear after a viral or bacterial infection, immunizations, exposure to a toxin, or in association with another illness such as lupus or HIV (human immunodeficiency virus).
Idiopathic thrombocytopenic purpura is usually not considered a disease that can be passed from one generation to another.
REFERENCES:
- Consolini R, Costagliola G, Spatafora D. The Centenary of Immune Thrombocytopenia-Part 2: Revising Diagnostic and Therapeutic Approach. Front Pediatr. 2017 Aug 21;5:179. doi: 10.3389/fped.2017.00179. PMID: 28871277; PMCID: PMC5566994.
- Kistangari G, McCrae KR. Immune thrombocytopenia. Hematol Oncol Clin North Am. 2013 Jun;27(3):495-520. doi: 10.1016/j.hoc.2013.03.001. PMID: 23714309; PMCID: PMC3672858.
- Neunert C, Terrell DR, Arnold DM, Buchanan G, Cines DB, Cooper N, Cuker A, Despotovic JM, George JN, Grace RF, Kühne T, Kuter DJ, Lim W, McCrae KR, Pruitt B, Shimanek H, Vesely SK. American Society of Hematology 2019 guidelines for immune thrombocytopenia. Blood Adv. 2019 Dec 10;3(23):3829-3866. doi: 10.1182/bloodadvances.2019000966. Erratum in: Blood Adv. 2020 Jan 28;4(2):252. PMID: 31794604; PMCID: PMC6963252.
- Provan D, Arnold DM, Bussel JB, Chong BH, Cooper N, Gernsheimer T, Ghanima W, Godeau B, González-López TJ, Grainger J, Hou M, Kruse C, McDonald V, Michel M, Newland AC, Pavord S, Rodeghiero F, Scully M, Tomiyama Y, Wong RS, Zaja F, Kuter DJ. Updated international consensus report on the investigation and management of primary immune thrombocytopenia. Blood Adv. 2019 Nov 26;3(22):3780-3817. doi: 10.1182/bloodadvances.2019000812. PMID: 31770441; PMCID: PMC6880896.
- Patel VL, Mahévas M, Lee SY, Stasi R, Cunningham-Rundles S, Godeau B, Kanter J, Neufeld E, Taube T, Ramenghi U, Shenoy S, Ward MJ, Mihatov N, Patel VL, Bierling P, Lesser M, Cooper N, Bussel JB. Outcomes 5 years after response to rituximab therapy in children and adults with immune thrombocytopenia. Blood. 2012 Jun 21;119(25):5989-95. doi: 10.1182/blood-2011-11-393975. Epub 2012 May 7. PMID: 22566601; PMCID: PMC3383014.
- Bussel J, Arnold DM, Grossbard E, Mayer J, Treliński J, Homenda W, Hellmann A, Windyga J, Sivcheva L, Khalafallah AA, Zaja F, Cooper N, Markovtsov V, Zayed H, Duliege AM. Fostamatinib for the treatment of adult persistent and chronic immune thrombocytopenia: Results of two phase 3, randomized, placebo-controlled trials. Am J Hematol. 2018 Jul;93(7):921-930. doi: 10.1002/ajh.25125. Epub 2018 May 15. PMID: 29696684; PMCID: PMC6055608.
- Mayo Clinic Staff. (2017). Idiopathic thrombocytopenic purpura (ITP). mayoclinic.com/health/idiopathic-thrombocytopenic-purpura/DS00844
- Neunert CE. Management of newly diagnosed immune thrombocytopenia: can we change outcomes? Blood Adv. 2017 Nov 14;1(24):2295-2301. doi: 10.1182/bloodadvances.2017009860. Erratum in: Blood Adv. 2018 Aug 14;2(15):1817. PMID: 29296878; PMCID: PMC5737126.
- Zufferey A, Kapur R, Semple JW. Pathogenesis and Therapeutic Mechanisms in Immune Thrombocytopenia (ITP). J Clin Med. 2017 Feb 9;6(2):16. doi: 10.3390/jcm6020016. PMID: 28208757; PMCID: PMC5332920.