Myasthenia gravis (MG) and Lambert Eaton syndrome (also known as Lambert Eaton myasthenic syndrome) are autoimmune neuromuscular disorders that affect muscle functions. These two muscle disorders are quite rare and can make simple tasks more challenging for individuals suffering from them. Because both conditions affect muscles, they are often misdiagnosed due to similarities in symptoms.
Speak to a Specialist
About Copay AssistanceTo provide a clear understanding to patients or their caregivers about these two neuromuscular disorders, we will briefly explain the key differences between myasthenia gravis (MG) vs. Lambert Eaton syndrome (LEMS).
The article will also discuss how both conditions differ in terms of cause, risk factors, affected body parts, onset and progression, diagnosis, and affected population.
What Is Myasthenia Gravis?
Myasthenia gravis is a chronic and relatively rare autoimmune disorder that causes muscle weakness and severe fatigue. This condition occurs when communication between your nerves and muscles becomes disturbed at the neuromuscular junction (an area where the nerve and muscle connect).
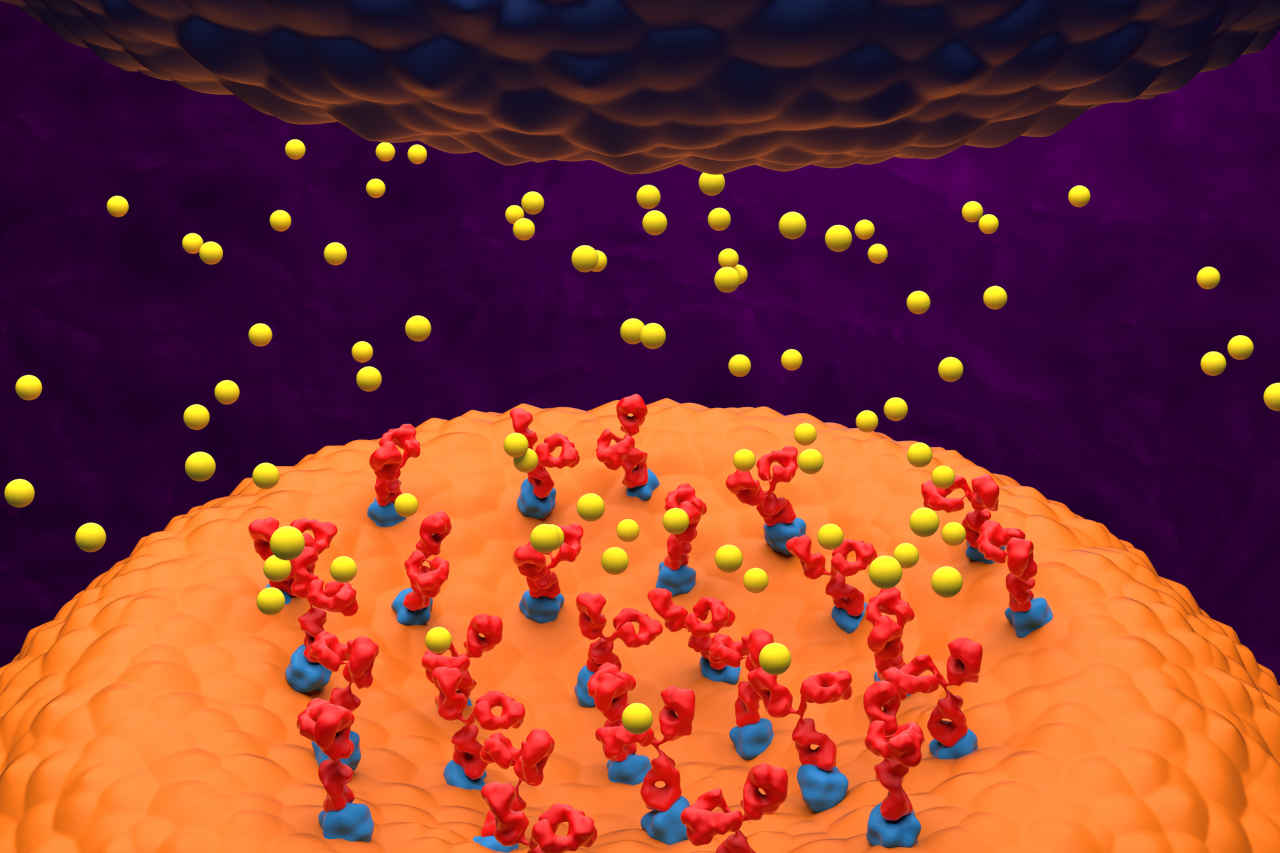
Normally, when a healthy person wants to move or lift something, the brain sends nerve impulses or signals. The nerve endings then release a substance called acetylcholine that attaches to its receptor on the skeletal muscle cell and causes a muscle contraction.
However, in people with MG, their immune system produces auto-antibodies that block or destroy the acetylcholine receptor sites at the neuromuscular junction and prevent muscle from contracting. Consequently, people with MG experience difficulty in performing tasks that require strong muscles, like lifting things and swallowing, etc.
What Is Lambert Eaton Myasthenic Syndrome?
Lambert Eaton myasthenic syndrome is a rare autoimmune disorder that also occurs due to a communication breakdown between your nerves and muscle cells at the neuromuscular junction. This disruption leads to the gradual onset of muscle weakness.
However, the mechanism of LEMS differs from MG. In this condition, auto-antibodies produced by the immune system block calcium channels on nerve endings. These channels are required for the release of acetylcholine from the nerve endings. When autoantibodies block these channels, less acetylcholine is released, which is insufficient to cause normal muscle contraction, and as a result, people with LEMS experience muscle weakness.
Myasthenia Gravis vs. Lambert Eaton Syndrome: Key Differences
Even though both neuromuscular diseases occur as a result of communication breakdown between nerves and the muscles at the neuromuscular junction, they are distinct in the following ways:
Causative Factors
The exact underlying cause of myasthenia gravis (MG) is still unknown. However, it is believed that a number of factors are involved in causing this condition, such as genetics, underlying disease (thymic tumor or thymoma), and immune factors.
On the other hand, Lambert Eaton myasthenic syndrome (LEMS) is mainly associated with an underlying disease called small lung cancer in about 50% – 60% of cases. It is thought that when the immune system fights the cancer cells, it also inadvertently attacks the nerve endings because cancer cells contain some of the same proteins that are also present in nerve endings.
However, normal individuals can also get LEMS, and in around 40% – 50% of cases, the cause is still unknown.
Onset and Progression
The onset of symptoms in individuals with MG can be sudden or gradual and the symptoms then progress over time. This condition first affects eye muscles and causes partial paralysis of eye movement. About half of the patients experience drooping eyelids (ptosis) or double vision (diplopia) as an initial symptom. Over time, muscle weakness spreads to other body parts, including facial, neck, and limb muscles, and could worsen if not treated in time.
On the other hand, LEMS patients have subacute onset. Unlike MG, which affects the eye muscle first, LEMS causes proximal muscle weakness in the lower limbs (upper legs and hips), which leads to difficulty walking.
With time, the muscle weakness temporarily improves after repetitive muscle activity, which is a unique feature of this condition.
Get Financial Assistance for Your Medications
Affected Populations
Myasthenia gravis and Lambert Eaton myasthenic syndrome can affect people of any age. However, MG is more prevalent in young women in their 20s or 30s and older men in their 60s or 70s. Conversely, LEMS is more common in middle-aged adults, especially those with small lung cancer and a history of smoking.
Diagnosis of Myasthenia Gravis vs. Lambert Eaton Syndrome

Healthcare providers follow a series of tests for the diagnosis of MG, including clinical evaluation (medical history and physical test), blood test (to check anti-acetylcholine receptor antibodies [AChR] or anti-muscle-specific kinase antibodies related to MG), electromyography (to measure muscle and nerve function), and, in some cases, imaging studies like a chest CT to check associated conditions, such as thymus gland abnormalities.
Like MG, clinical evaluation, electromyography, and blood tests (to check voltage-gated calcium channel antibodies) are also used in the case of LEMS diagnosis. Sometimes, a CT scan is also recommended to check underlying associated disorders, such as small-cell lung cancer in patients.
Treatment Procedures for MG and LEMS
Though there is no cure for MG and LEMS, several different treatment strategies and medications can help reduce disease-associated symptoms in patients.
- In the case of MG, acetylcholinesterase inhibitors, corticosteroids, or immunosuppressive agents are prescribed.
- For LEMS, immunoglobulin therapy, plasmapheresis, medication (such as amifampridine and pyridostigmine), and immunosuppressant agents are used.
Conclusion
Myasthenia gravis and Lambert Eaton myasthenic syndrome are two autoimmune diseases that impact muscle functions and cause muscle weakness. While both diseases share similarities in symptoms, they differ in cause, risk factors, onset and progression, diagnosis and treatment, and the population they predominantly affect. Understanding the key differences between these two medical conditions can help patients and healthcare providers ensure accurate diagnosis and timely management.
REFERENCES:
- Pascuzzi, R. M., & Bodkin, C. L. (2022). Myasthenia Gravis and Lambert-Eaton Myasthenic Syndrome: New Developments in Diagnosis and Treatment. Neuropsychiatric Disease and Treatment, 18, 3001-3022. https://doi.org/10.2147/NDT.S296714
- Wirtz, P. W., Sotodeh, M., Nijnuis, M. G., Van Doorn, P., Van Engelen, B., Hintzen, R., De Kort, P. L., Kuks, J. B. M., Twijnstra, A., Visser, M., Visser, L. H., Wokke, J. H. J., Wintzen, A. R., & Verschuuren, J. J. (2002). Difference in distribution of muscle weakness between myasthenia gravis and the Lambert-Eaton myasthenic syndrome. Journal of Neurology, Neurosurgery, and Psychiatry, 73(6), 766–768. https://doi.org/10.1136/jnnp.73.6.766
- Lambert-Eaton Myasthenic Syndrome (LEMS) – Diseases | Muscular Dystrophy Association. (2023, August 16). Muscular Dystrophy Association. https://www.mda.org/disease/lambert-eaton-myasthenic-syndrome
- Jayarangaiah, A. (2022, July 12). Lambert-Eaton Myasthenic Syndrome. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK507891/
- Myasthenia gravis – Symptoms and causes – Mayo Clinic. (2023, June 22). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/myasthenia-gravis/symptoms-causes/syc-20352036
- Dresser, L., Wlodarski, R., Rezania, K., & Soliven, B. (2021). Myasthenia gravis: epidemiology, pathophysiology and clinical manifestations. Journal of Clinical Medicine, 10(11), 2235.
- Ivanovski, T., & Miralles, F. (2019). Lambert-Eaton Myasthenic syndrome: early diagnosis is key. Degenerative Neurological and Neuromuscular Disease, 27-37.
- Lee, J. H., Baek, S. K., Han, J. J., Kim, H. J., Lee, Y. A., Yoo, D., & Maeng, C. H. (2022). Lambert-Eaton myasthenic syndrome (LEMS) in a patient with lung cancer under treatment with pembrolizumab: a case study. Journal of Chemotherapy, 1-6.