This article answers the 10 most common questions about Kawasaki disease. Empower yourself with evidence-based health information to make better choices.
Highlights
- Kawasaki disease (KD) is a rare condition that usually affects children younger than 5. Older children and adults rarely get KD.
- KD causes the blood vessels to become inflamed. Typical symptoms include fever, rash, and a red strawberry tongue.
- What causes Kawasaki disease is unknown. Researchers are studying the possible role of genetics and environmental factors, such as infections.
- Diagnostic criteria involve the presence of symptoms such as fever, rash, strawberry tongue, and others.
- Prompt treatment, with high-dose IVIG and aspirin, results in complete recovery in most children.
What Is Kawasaki Disease?
Kawasaki Disease is also called Kawasaki syndrome or mucocutaneous lymph node syndrome.
Kawasaki disease is a form of vasculitis, which is inflammation of the blood vessels. Inflamed blood vessels cannot supply enough blood to tissues and organs. Moreover, they become weak and prone to tearing.
KD causes swelling of the blood vessels throughout the body. But heart complications are most likely when blood vessels that supply the heart (coronary arteries) get affected. KD is one of the leading causes of heart disease in children in the US.
KD isn’t contagious, though there have been reports of occasional community-wide outbreaks.
How Common Is Kawasaki Disease?
According to the Centers for Disease Control and Prevention (CDC), KD affects about 9 to 20 per 100,000 children younger than 5 in the US. In contrast, 50 to 250 per 100,000 children in Japan, Taiwan, or Korea develop KD [1,2].
In 2016, out of 5,440 KD-related hospitalizations in children under 18, 3,935 involved children younger than 5 [1].
What Causes Kawasaki Disease?
Experts are yet to identify what exactly causes Kawasaki disease. However, initial research suggests it might be linked to genes, viruses, bacteria, and environmental triggers like irritants.
Recent studies show that carrying specific genetic changes may make your child more likely to get KD. Having a sibling with KD may increase the risk severalfold. In addition, over 4 in 10 children diagnosed with KD have a viral respiratory infection [3].
Who Gets Kawasaki Disease?
Kawasaki disease occurs most often in children between 6 months and 5 years of age. Older children, children younger than 4 months, and adults rarely get KD.
In a 2015 case report, Japanese researchers reported a very rare case of KD in a 37-year-old Japanese man [4]. Talk to your doctor if you have a fever with no known cause and rash, especially if you have a current or recent history of a viral infection.
Other factors that may increase the risk of KD include:
- Sex: Boys are more likely than girls to develop KD and its complications, including death.
- Ethnicity: Children of Asian descent, particularly Japanese, are at the highest risk.
- Seasonality: KD is more likely to occur in the winter and spring months.
Kawasaki Disease and COVID-19: Is There a Link?
Available studies haven’t found a link between KD and COVID-19.
In some children, COVID-19 may cause a condition with symptoms that resemble KD. Doctors call this condition multisystem inflammatory syndrome in children (MIS-C).
MIS-C may also cause additional symptoms, such as:
- Abdominal pain
- Nausea
- Vomiting
- Diarrhea
- Headaches
- Low blood pressure
While Kawasaki disease typically occurs in children, MIS-C can affect both children and adolescents.
What Are the Symptoms of Kawasaki Disease?

Kawasaki disease occurs suddenly, and symptoms appear in phases.
Phase 1 Symptoms
- High fever (over 101°F) that lasts more than 5 days and doesn’t improve with medications
- Rash on the trunk and in the genital area
- Bloodshot eyes with no thick discharge
- Strawberry tongue
- Red, swollen skin on the palms and soles
- Swollen lymph nodes in the neck
Phase 2 Symptoms
Phase 2 symptoms may include:
- Skin peeling on the tips of the fingers and toes
- Joint pain
- Diarrhea
- Vomiting
- Abdominal pain
Phase 3 Symptoms
During the third phase, the signs and symptoms will go away slowly. It might last up to 8 weeks. Your child may show symptoms of tiredness, irritability, and low energy.
How Is KD Diagnosed?
No specific diagnostic test for KD exists. Your child’s doctor will make a diagnosis based on the symptoms and physical exam.
The diagnostic criteria for KD is a fever lasting over 5 days and having at least 4 of the following 5 features [5]:
- Strawberry tongue
- Rash
- Bloodshot eyes with no thick discharge
- Swollen, red skin on the palms of the hands and the soles of the feet
- Swollen lymph nodes in the neck
Incomplete or atypical KD is when children don’t fulfill the usual criteria for KD diagnosis but still have the disease.
How Is Kawasaki Disease Treated?
Prompt treatment is crucial to reduce the risk of complications. Children who stay in the hospital for treatment usually receive:
Aspirin
Your child will receive moderate to high dose aspirin until fever subsides. Then, a low dose is given for up to 8 weeks.
IVIG
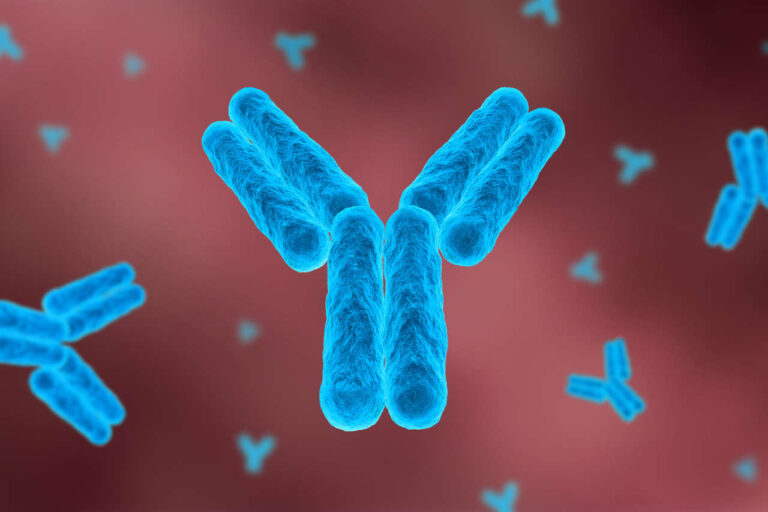
Timely treatment with IVIG can greatly lower the risk of heart complications. IVIG contains proteins called antibodies. These proteins can stop your immune system from attacking the blood vessels.
Corticosteroids
Corticosteroids may be an option for children who don’t respond to IVIG.
What Are the Complications of Kawasaki Disease?
Potential complications include:
- Aneurysms (bulging in the wall of a blood vessel)
- Abnormal heart rhythm
- Blood clots (may lead to heart attacks)
- Swelling of the coronary arteries
- Heart valve problems
What Is the Life Expectancy for Someone with KD?
If blood vessels in the heart aren’t affected, full recovery is possible. Heart attack due to aneurysms is the main cause of death.
Lifelong monitoring is necessary in children with aneurysms or other heart complications.
According to a 2022 review, survival ranges from 92% to 99% at 10 years and 85% to 99% at 20 years [6].
Get Financial Assistance
REFERENCES:
- About Kawasaki Disease | Kawasaki Disease | CDC. www.cdc.gov/kawasaki/about.html.
- Owens AM, Plewa MC. Kawasaki Disease. [Updated 2023 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537163/
- Turnier, Jessica L et al. “Concurrent Respiratory Viruses and Kawasaki Disease.” Pediatrics vol. 136,3 (2015): e609-14. doi:10.1542/peds.2015-0950
- Ueda Y, Kenzaka T, Noda A, Yamamoto Y, Matsumura M. Adult-onset Kawasaki disease (mucocutaneous lymph node syndrome) and concurrent Coxsackievirus A4 infection: a case report. Int Med Case Rep J. 2015;8:225-230 https://doi.org/10.2147/IMCRJ.S90685
- Morishita, Kimberly A, and Ran D Goldman. “Kawasaki disease recognition and treatment.” Canadian family physician Medecin de famille canadien vol. 66,8 (2020): 577-579.
- Lee, J. J., Lin, E., Widdifield, J., Mahood, Q., McCrindle, B. W., Yeung, R. S. M., & Feldman, B. M. (2022). The Long-term Cardiac and Noncardiac Prognosis of Kawasaki Disease: a Systematic review. Pediatrics (Evanston), 149(3). https://doi.org/10.1542/peds.2021-052567