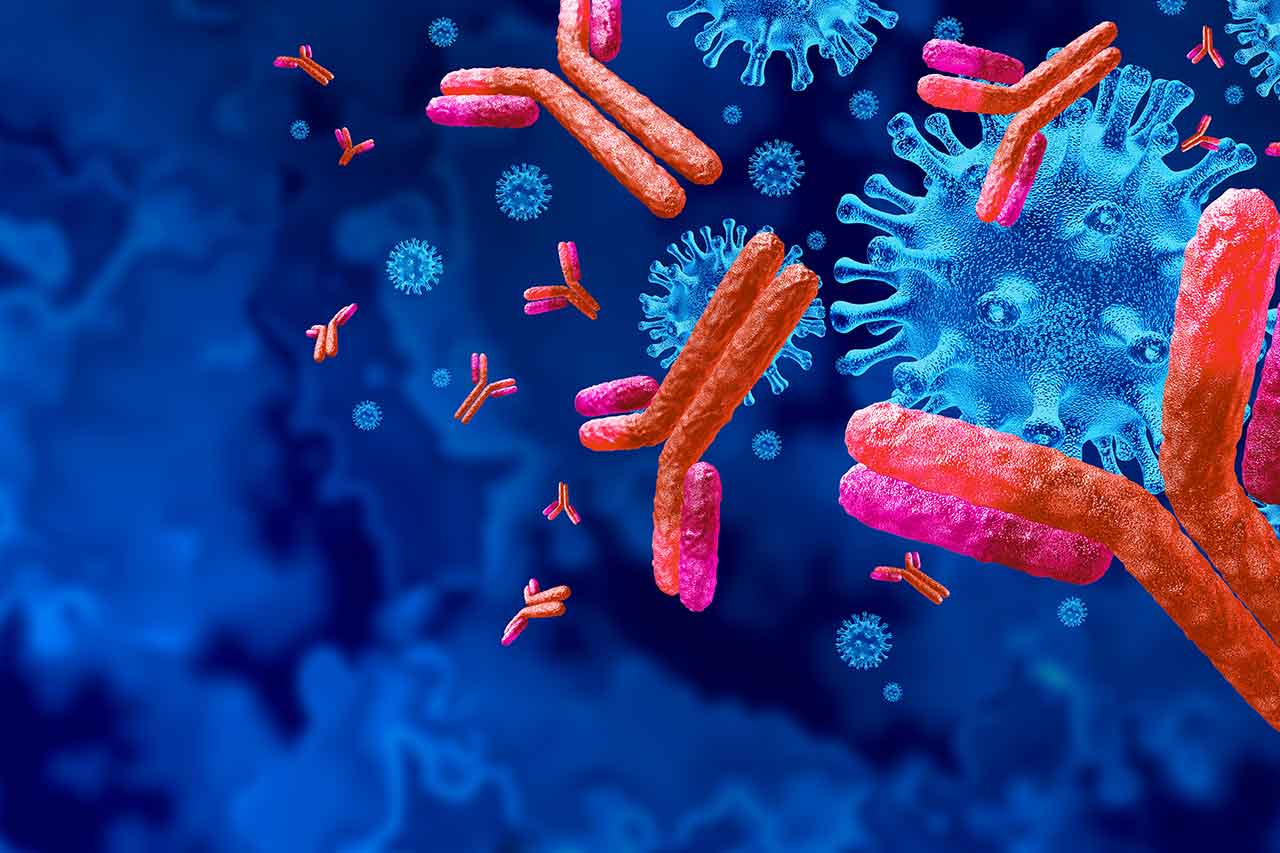
Immunoglobulins are proteins made in the body that serve as antibodies. These proteins are a crucial part of the immune system as they identify and incapacitate any foreign substance in the body, such as bacteria and viruses. They form part of humoral immunity, which is mediated by B-cells, a type of white blood cell.
Can IVIG help?
Free IVIG Treatment InfoImmunoglobulins consist of five major classes: immunoglobulin G (IgG), immunoglobulin A (IgA), immunoglobulin M (IgM), immunoglobulin D (IgD), and immunoglobulin E (IgE). The most abundant class in the blood is IgG, which comprises approximately 75% of all antibodies in the body. Any form of IgG deficiency or IgG subclass deficiency can have a significant impact on a person’s immunity.
How Do Immunoglobulins Work?
The purpose of immunoglobulins is mainly to fight off and protect the body from infections. Once any type of germ enters the body, B-cells react by releasing immunoglobulins. Initially, immunoglobulin M is released, but eventually, immunoglobulin G is produced in bulk.
Immunoglobulin G captures invading germs which are then engulfed by larger white blood cells called macrophages. The B-cells will then “remember” the look of the germ, and the body will be ready to fight the germ more quickly the next time it enters the body. This ability will be impaired in people with IgG deficiency or IgG subclass deficiency.
What Role Does IgG Play in the Body?
Like the other antibodies, IgG fights off and prevents infections, but specifically, its role is more reserved for the “secondary immune response.” When a person is exposed to the same type of infection the second time around, there is already a large number of IgG antibodies in circulation, ready to neutralize the bacteria, virus, or fungi. Since IgG has further subclasses, it can perform several other functions as well, such as:
- Activating the complement system (which enhances the abilities of antibodies and macrophages)
- Neutralization of toxins
- Playing a role in antibody-dependent cell-mediated cytotoxicity (ADCC), where cells marked by IgG antibodies are broken down by T-cells
- Being associated with hypersensitivity or allergic reactions.
Any form of IgG deficiency or IgG subclass deficiency would lead to loss of the aforementioned functions in addition to an inability to prevent infections. Furthermore, IgG is the only antibody that can pass through the placenta, thereby providing protection to a fetus still in the womb. It also passes through breast milk to the infant. This means that Immunoglobulin G forms a critical part of the immunity of a child during the first 6 months.
The child will have the same amount of antibodies as the mother and this will keep the child secure from recurrent infections.
What Happens to the Body if Immunoglobulins Are Low, Specifically for IgG?
Healthcare providers consult different labs that have different ranges for normal levels, but generally, for older children and adults, the range is 6.0 – 16.0 g/l. Levels in an infant are comparatively lower and take time to reach the range of adults. IgG subclass levels are highly variable, even for the same individual at different ages. IgG2 is virtually absent in children less than 2 years of age. This is normal and not considered an IgG subclass deficiency.
Anything less than the aforementioned range is termed IgG deficiency, and a person may need regular transfusions. Low amounts of circulating IgG in the intravascular or extravascular space of the body will result in frequent or severe infections, especially from the same type of bacteria, virus, or fungi. This happens if there are too few B-cells in the body, the B-cells are not producing the appropriate amount of immunoglobulins, or the immunoglobulins produced themselves are defective.
Low IgG levels, together with a normal IgA and normal IgM level, do not necessarily mean there is IgG deficiency. The specific antibody response needs to be evaluated to determine diagnosis and treatment.
For the sake of simplicity, IgG deficiency is divided into two categories:
- Selective, where only IgG levels are low (or IgG subclass).
- Non-selective, where all immunoglobulins are affected.
Get Your IVIG Dose
At-Home InfusionIs IgG Deficiency Rare?
Although the frequency of IgG deficiency and all its subclasses (IgG1, IgG2, IgG3, and IgG4) is not known, deficiencies in a specific subclass are considered more common and probably associated with diseases like common variable immunodeficiency (CVID).
What Exactly Causes This?
It is still unknown what exactly causes IgG deficiency, but the current theory held by healthcare providers is that people with IgG deficiency may have a lack or absence of certain genes, which can cause a failure to produce important components of the immune system. Some examples of diseases that cause IgG deficiency are:
- X-linked agammaglobulinemia (Bruton disease), where there are too few B-cells by birth.
- Transient hypoglobulinemia, where there is a temporary drop in immunoglobulin levels.
- Severe combined immunodeficiency (SCID), where there are absent or non-functional B and T cells.
- Thymoma, where there is a tumor of the thymus (a gland located within the chest that produces T-cells).
How Does One Know if a Person May Have IgG Deficiency?
If a person has recurrent or severe infections, particularly respiratory tract infections, or if lab tests repeatedly show the same bacteria/virus in cultures, this hints towards an immune deficiency, and the patient should be seen by a healthcare provider.
There is usually a pattern of infections observed in people with IgG deficiency, such as sinusitis (sinus infection), otitis media (middle ear infection), pharyngitis (throat infection), rhinitis (nasal cavity infection), or even contagious diseases like COVID-19.
On the other hand, a person may be completely normal or just have general symptoms of fever and headache if just a single subclass of IgG is deficient or absent such as in IgG2 deficiency. Such a person cannot be diagnosed as having IgG deficiency or IgG subclass deficiency until the specific clinical response of that subclass is elicited due to a particular infection.
What Diseases Manifest Due to IgG Deficiency?
People with IgG deficiency commonly experience recurring respiratory infections. Some of these include:
- Sinusitis (sinus infection)
- Otitis media (middle ear infection), associated with symptoms of fullness in the ear
- Rhinitis (infection of nasal cavity), associated with symptoms of nasal discharge
- Pharyngitis (throat infection), associated with symptoms of pain during swallowing
- Pneumonia (lung infection), associated with symptoms of breathlessness
- Bronchitis (infections of bronchus and/or bronchioles that lead into the lungs)
- Laryngitis (infection of larynx or voice box), associated with symptoms of hoarseness of voice
What Tests Can Be Performed To Check IgG Levels?
IgG levels can be measured by using ELISA (enzyme linked-immunosorbent assay), a medical test that is used to measure proteins, antibodies, and even hormones. As far as measuring IgG subclasses is concerned, many medical experts do not give significance to the levels; however, there is a clinical relevance to each subclass.
For example, patients infected with diphtheria who fail to produce antibodies may have a diagnosis of IgG1 deficiency. Patients with pneumococcal infections who fail to produce antibodies may have a diagnosis of IgG2 deficiency.
Other tests done on patients that may act as indicating signs include:
- Pulmonary function tests to assess whether the health of the lungs is normal.
- Radiographic studies such as X-rays to visualize sinusitis or bronchiectasis.
- Cultures to confirm the presence of a germ that is a repeat offender.
Get IVIG Copay Assistance
IVIG Financial AssistanceWhat Is the Treatment for Low IgG Levels?
There is no medicinal treatment or vaccine as such, but patients of IgG deficiency and IgG subclass deficiency are given a transfusion of immunoglobulins prepared from a pool of plasma obtained from many donors. After confirming the absence of potential infectious diseases from the donors, the plasma then undergoes numerous steps to make it pure from plasma cells and any harmful agent that may be life-threatening. The treatment is called intravenous immunoglobulin replacement therapy (IVIG therapy).
Although in the past, IgG was injected into the muscle or under the skin, nowadays, the ideal form of immunoglobulin replacement therapy is directly into the blood of patients to avoid serious complications.
There are certain prerequisites before initiating therapy. Firstly, if a patient has an active infection, then that infection must be managed with antibiotic treatment. Secondly, the patient must take prophylactic medicine, which is an extended duration of antibiotic treatment to prevent the recurrence of symptoms. Thirdly, if there is any pulmonary injury, then this should be managed, as any structural damage to the lungs can increase the chances of re-infection. Therapy should only start after all of these prerequisites are met.
What Are the Dosing and Schedule for IgG Transfusions?
IgG replacement doses are similar in all types of immunodeficiencies mainly because IgG subclass doses have not been made. The current preparation consists of almost 99% IgG with lower amounts of IgA, IgM, IgD, and IgE. The half-life is about 3 – 4 weeks, which means that the total amount of injected IgG will be reduced to half within 20 – 28 days.
The dosing schedule is given below:
- 300 – 600 mg/kg intravenously once every 3 to 4 weeks, or
- 100 – 200 mg/kg subcutaneously once a week
Is the Treatment Completely Safe?
The side effects of the treatment are not directly because of the IgG itself (or even IgG subclasses like IgG2) but due to transfusion-related adverse effects. One can expect the following during the process of infusion:
- Local site reactions
- Fatigue and low energy
- Headaches
- Muscle ache
- Fever and chills
These adverse effects are more common during the first infusion. Subsequent transfusions have lower rates of side effects.
One medical safety protocol is to ensure that the infusion is not faster than 0.01 ml/kg/min. Patients should be closely monitored. If symptoms emerge, then the transfusion should be temporarily stopped. Other measures include giving antipyretics, anti-histamines, or even corticosteroids before initiating transfusion.

How Can I Increase My IgG Levels?
Since antibodies are proteins, it’s no surprise that a diet lacking in this macronutrient leads to a weakened immune state; hence, foods like meat, fish, and eggs are essential in a balanced diet.
Another important factor is emotional state, or to be precise, stress. Research has proven an inverse correlation between stress and immunoglobulin levels. That is because stress causes the elevation of a hormone known as cortisol (which is a corticosteroid), and this suppresses the body’s antibodies.
REFERENCES:
- https://www.ncbi.nlm.nih.gov/books/NBK513460/
- https://www.gov.nl.ca/hcs/files/bloodservices-resources-pdf-adult-invig-inf-table.pdf
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/igg-deficiencies#:~:text=What%20causes%20IgG%20deficiencies%3F,linked%20to%20another%20immunoglobulin%20deficiency.
- https://www.niaid.nih.gov/diseases-conditions/common-variable-immunodeficiency-cvid#:~:text=Common%20variable%20immunodeficiency%20(CVID)%20is,also%20can%20occur%20in%20children.
- https://www.ncbi.nlm.nih.gov/books/NBK448170/#:~:text=Bruton%20agammaglobulinemia%2C%20also%20known%20as,antibody%20deficiency%20and%20recurrent%20infections.