
Pregnancy is an exciting and transformative journey for many women. However, if a woman has a pre-existing medical condition like chronic inflammatory demyelinating polyneuropathy (CIDP), then this condition may bring complications to the pregnancy.
Speak to a Specialist
About Copay AssistanceCIDP is a rare neurological disorder that affects the nerves in the body and causes coordination problems and progressive muscle weakness. The symptoms of CIDP can become worse if this condition is not managed properly, specifically during pregnancy.
For instance, one study reviewed 61 women of childbearing age with CIDP and reported that pregnant women tend to have a higher risk of relapses throughout the pregnancy, especially during the third trimester. Therefore, it is important to understand how CIDP can impact pregnancy.
In this article, we’ll explore what you need to know about CIDP and pregnancy, including precautions to take and potential complications to be aware of.
Understanding CIDP
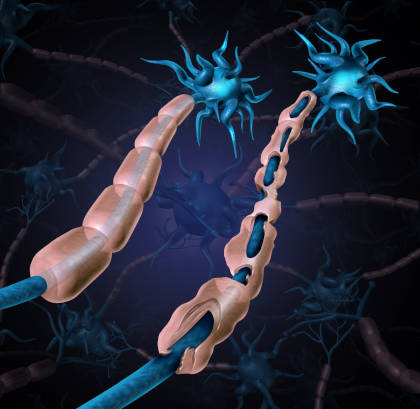
Chronic inflammatory demyelinating polyneuropathy is a rare autoimmune neurological condition in which the immune system mistakenly attacks and damages the peripheral nerves. Peripheral nerves are the network of nerves that connect your brain with the rest of the body organs and play a crucial role in controlling muscle movement and coordination.
However, in a person with CIDP, the immune system attacks the protective covering of these nerves called the myelin sheath. The damage to the myelin sheath slows down the ability of nerves to send signals and results in a wide range of symptoms such as progressive muscle weakness, pain, numbness, tingling sensation in arms and legs, loss of balance, difficulty walking, and fatigue.
CIDP and Pregnancy: Link Between the Two
The connection between CIDP and pregnancy is quite complex and not yet fully understood due to the limited number of studies. However, based on some case reports, it has been observed that pregnancy can trigger typical CIDP in women.
Normally, during pregnancy, a woman’s body undergoes a massive adaptation. The body not only experiences hormonal changes but also experiences a significant shift in the balance of immune cells to tolerate the developing fetus. This altered immune state might lead to the onset of CIDP symptoms.
On the other hand, when women with diagnosed CIDP become pregnant, the risk of relapses increases throughout gestation due to pregnancy-related immune system alterations.
Complications That Women With CIDP May Face During Pregnancy
Many women with CIDP can have successful pregnancies and healthy babies, but there are some potential complications that some women with CIDP face:
Risk of Relapses or Periodic Flare-Ups
During pregnancy, the risk of CIDP relapses or periodic flare-ups, which are periods of worsened symptoms, becomes more frequent, leading to increased weakness and disability. Since pregnancy influences the immune system, it also largely impacts disease activity and the clinical course of CIDP in women.
For instance, a retrospective study of nine pregnant women with CIDP revealed that pregnant women experienced their symptoms worsening in the third trimester.
Not all women experience an increase in CIDP-related symptoms during pregnancy. Some women might see an improvement in their condition.
Postpartum Period
The postpartum period is the period that begins after giving birth, when your body returns to the non-pregnant stage. Like the third trimester, the postpartum period also carries the highest risk of symptom worsening. This exacerbation can occur due to fatigue, hormonal changes, and stress.
Neonatal Complications
Though CIDP does not directly affect the developing fetus, there are rare chances that the mother’s antibodies may affect the fetus’s nerves by crossing the placenta. This condition is known as congenital CIDP.
Medication Risks
Sometimes, CIDP patients require ongoing treatment to manage their condition. Certain medications are used during the CIDP clinical course, which may not be suitable for developing babies. For instance, some of the immunosuppressive medications and steroid-sparing therapy, such as azathioprine (category D), are usually not recommended during pregnancy as they could potentially harm the fetus.
Labor and Delivery Challenges
Since CIDP affects the nerves involved in muscle movement, it sometimes becomes difficult for mothers to deliver babies vaginally due to weakness of the muscle.
Treatment Info
Get Prior AuthorizationManaging CIDP Symptoms and Pregnancy Complications
With supportive care, careful planning, and certain precautions, many women with CIDP can manage their symptoms during pregnancy. Some of the key points you may consider to ensure the well-being and safety of the baby throughout pregnancy include the following:
- Consult a neurologist as they can help you adjust your treatment plan and medication based on your CIDP state and symptoms severity.
- Maintain regular neurologist and prenatal checkups.
- Consider physical therapy to help manage muscle weakness and coordination.
- Discuss labor and delivery possibilities with your healthcare provider in advance to avoid complications in the future.
Hence, it is essential to work closely with your healthcare provider if you have CIDP and are expecting. This way, your provider can help ensure the best possible outcomes for you and your baby.
REFERENCES:
- Kim, W., Kim, J. H., Bae, D. W., & An, J. Y. (2021). Postpartum attacks of acute-onset chronic inflammatory demyelinating polyneuropathy in a young woman with successive pregnancies. Quantitative Imaging in Medicine and Surgery, 11(11), 4683-4686. https://doi.org/10.21037/qims-21-177
- Weimer, L. H. (2019). Neuromuscular disorders in pregnancy. Handbook of Clinical Neurology, 172, 201-218. https://doi.org/10.1016/B978-0-444-64240-0.00012-X
- Silwal, A., Pitt, M., Phadke, R., Mankad, K., Davison, J. E., Rossor, A., DeVile, C., Reilly, M. M., Manzur, A. Y., Muntoni, F., & Munot, P. (2018). Clinical spectrum, treatment and outcome of children with a suspected diagnosis of chronic inflammatory demyelinating polyradiculoneuropathy. Neuromuscular Disorders, 28(9), 757-765. https://doi.org/10.1016/j.nmd.2018.06.001
- Kohle, F., Kuwabara, S., & Lehmann, H. C. (2021). Chronic inflammatory demyelinating polyneuropathy and pregnancy: systematic review. Journal of Neurology, Neurosurgery & Psychiatry, 92(5), 473-478. http://dx.doi.org/10.1136/jnnp-2020-325321
- Manley, C., & Geary, F. (2017). An Incidence of Chronic Inflammatory Demyelinating Polyneuropathy in Pregnancy [28L]. Obstetrics & Gynecology, 129(5), S128-S129. Doi: 10.1097/01.AOG.0000514659.74781.24
- Thaisetthawatkul, P., & Logigian, E. (2018). Guillain-Barré Syndrome and Chronic Inflammatory Demyelinating Polyradiculoneuropathy in Pregnancy. https://doi.org/10.1093/med/9780190667351.003.0026












