
Though both chronic inflammatory demyelinating polyneuropathy (CIDP) and multiple sclerosis (MS) cause damage to the nerves and can coexist in rare cases, they are different diagnoses.
Speak to a Specialist About
Copay AssistanceIn this article, you will learn about the key differences between CIDP and MS in terms of causes, risk factors, treatment options, and more. Also, you will find answers to seven frequently asked questions about CIDP vs. MS.
An Overview of CIDP and MS
CIDP is a rare, long-lasting neurological disorder. It causes progressive weakness and impaired senses in the arms and legs.
Signs and symptoms can include:
- Tingling in the arms and legs
- Gradual weakening of the arms and legs
- Absence of reflexes, such as the knee-jerk reaction
- Loss of balance
- Unsteady walk
- Difficulty walking or climbing stairs
- Falls
- Reduced feeling in the arms and legs (usually starting with an inability to feel a pin prick)
- Fatigue
- Unusual feelings in the body
- Spontaneous pain (occasionally)
Multiple sclerosis is a chronic (long-lasting), unpredictable disease. It affects your brain, spinal cord, and optic nerves (nerves that send signals to your brain).
Symptoms can include:
- Fatigue
- Vision problems
- Numbness and tingling
- Muscle spasms, stiffness and weakness
- Mobility problems
- Pain
- Problems with thinking, learning, and planning
- Depression and anxiety
- Sexual problems
- Bladder problems
- Bowel problems
- Speech and swallowing difficulties
CIDP vs. MS: Number of People Affected
CIDP is far less common than MS.
Estimates suggest about 30,000 Americans have CIDP [1]. Moreover, men are twice as likely as women to get CIDP [2]. In contrast, Nearly 1 million Americans live with MS, and it is three times more common in women than in men [3,4].
Treatment Info
Get Prior AuthorizationCIDP vs. MS: Cause
Both CIDP and MS are not inherited and have no known cause.
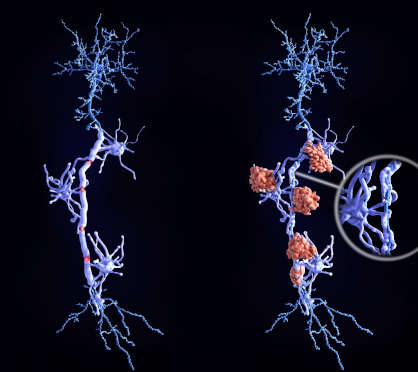
In people with CIDP, their immune systems attack myelin (the fatty layer that protects the nerve fibers) in the peripheral nerves. Peripheral nerves lie outside your brain and spinal cord.
In people with MS, their immune systems attack myelin in the brain and spinal cord.
Risk Factors
Several studies have associated CIDP variants with certain cancers, HIV infections, and a long history of type 2 diabetes.
The risk factors for MS include:
- Age (between 20 and 40 years)
- Family history
- Epstein-Barr virus infection
- Smoking
- Obesity
- Low vitamin D levels
- Being White
- Type 1 diabetes
- Inflammatory bowel disease (IBD)
Some people believe that exposure to heavy metals or organic solvents can trigger MS. However, this is unproven.
Treatment Options
CIDP treatment aims to reverse or stop nerve damage. Some people can get their normal nerve function back with treatment. In cases when nerve function cannot be restored, treatment aims at preventing the symptoms from getting worse.
Treatment options for CIDP include:
- Corticosteroids: They reduce nerve swelling and improve symptoms.
- Plasmapheresis: Also called plasma exchange, this treatment removes antibodies (proteins causing your symptoms) from your blood.
- IVIG: Intravenous immune globulin, or IVIG, uses antibodies from donors to counteract the effects of antibodies responsible for your symptoms.
- Immunosuppressants: These medications prevent your immune system from attacking the myelin sheath. Examples include azathioprine (Imuran), cyclophosphamide (Cytoxan), cyclosporine (Sandimmune), etanercept (Enbrel), and methotrexate (Otrexup, Rheumatrex).
Rituximab, a monoclonal antibody, has shown promise in improving symptoms. However, the U.S. FDA has not yet approved this drug for CIDP.
The first-line treatments for MS are [5]:
- Interferon beta (IFNB)
- Glatiramer acetate (GA)
- Dimethyl fumarate
Those who fail to respond to first-line therapies may receive one of the following drugs:
- Alemtuzumab
- Fingolimod
- Natalizumab
Consult a Specialist
Get Copay AssistanceCIDP vs. MS: Prognosis
Early treatment is crucial to improve the chances of limiting symptoms. Without treatment, your symptoms will likely worsen. Left untreated, 33% of people with CIDP will need a wheelchair.
Moreover, 13-24% of people have severe disabilities despite treatment, and nearly 40% of them need continuous immunosuppressant therapy [6].
CIDP is unlikely to affect life expectancy, provided you get the right treatment.
Living with MS can be challenging. While MS is rarely fatal, severe disease can lead to complications, such as swallowing difficulties.
Thankfully, medical advances have dramatically increased survival in people with MS. According to a large study, median life expectancy was 74.7 years for MS and 81.8 years for the general population [7].
CIDP vs. MS: Frequently Asked Questions
What is the difference between CIDP and multiple sclerosis?
MS damages the nerves of your central nervous system (brain, spinal cord, and optic nerves). On the other hand, CIDP affects the nerves that are present outside your central nervous system.
Can MS be confused with CIDP?
CIDP is often underdiagnosed or misdiagnosed, as it is rare and shares several features with other conditions, such as MS and Guillain-Barré syndrome (GBS).
Is CIDP related to MS?
It is unclear if CIDP and MS are related, though they can coexist. What we currently know is both diseases damage your nerves.
What is a new treatment for CIDP?
In February 2021, the U.S. FDA approved Pfizer’s Panzyga (IVIG) to treat adults with CIDP. Panzyga is the first and only FDA-approved IVIG with two maintenance dosing options to treat CIDP.
Why is CIDP hard to diagnose?
Two reasons make CIDP hard to diagnose. First, it is very rare. Second, many other disorders have similar symptoms. Examples include MS, GBS, Lewis-Sumner syndrome, and Charcot-Marie-Tooth disease.
Can you fully recover from CIDP?
Full recovery is unlikely because no cure exists. Even if it happens, a person will typically experience symptoms like numbness for the rest of their life. Interestingly, Austrian researchers reported a unique (and probably the only) case of a male who recovered fully with ocrelizumab. Note that the person had coexisting MS [8].
What is the success rate of CIDP treatment?
The success rate of CIDP treatment can vary widely depending on several factors. However, based on available evidence, it is safe to say that nearly half of all people with CIDP have significant improvement without disability.
REFERENCES:
- School, McGovern Medical. “CIDP | Chronic Inflammatory Demyelinating | UTHealth Houston.” Neurology, Neurosurgery, Spine Care | UTHealth Neurosciences, 17 Oct. 2023, med.uth.edu/neurosciences/conditions-and-treatments/nerve-disorders/chronic-inflammatory-demyelinating-polyneuropathy.
- Gogia B, Rocha Cabrero F, Khan Suheb MZ, et al. Chronic Inflammatory Demyelinating Polyradiculoneuropathy. [Updated 2023 Jun 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563249/
- “MS Prevalence.” National Multiple Sclerosis Society, www.nationalmssociety.org/About-the-Society/MS-Prevalence#.
- “Women Living With Multiple Sclerosis.” National Multiple Sclerosis Society, www.nationalmssociety.org/What-is-MS/Who-Gets-MS/Women-with-MS#.
- Gajofatto, Alberto, and Maria Donata Benedetti. “Treatment strategies for multiple sclerosis: When to start, when to change, when to stop?.” World journal of clinical cases vol. 3,7 (2015): 545-55. doi:10.12998/wjcc.v3.i7.545
- Baek, Seol-Hee. “Insight Into the Prognostic Factors of Chronic Inflammatory Demyelinating Polyneuropathy.” Annals of Clinical Neurophysiology, vol. 22, Apr. 2020, p. 8. https://doi.org/10.14253/acn.2020.22.1.8.
- Lunde, Hanne Marie Bøe et al. “Survival and cause of death in multiple sclerosis: a 60-year longitudinal population study.” Journal of neurology, neurosurgery, and psychiatry vol. 88,8 (2017): 621-625. doi:10.1136/jnnp-2016-315238
- Auer, Michael et al. “Recovery of Chronic Inflammatory Demyelinating Polyneuropathy on Treatment With Ocrelizumab in a Patient With Co-Existing Multiple Sclerosis.” Journal of central nervous system disease vol. 14 11795735221084837. 28 Mar. 2022, doi:10.1177/11795735221084837












