- Bệnh nhược cơ là một rối loạn tự miễn dịch gây ra tình trạng yếu cơ do sự suy giảm khả năng giao tiếp giữa thần kinh và cơ.
- Tuổi tác và giới tính là những yếu tố nguy cơ chính gây bệnh nhược cơ vì bệnh thường ảnh hưởng đến phụ nữ trẻ (<40) và nam giới lớn tuổi (>60) nhiều hơn.
- Các bệnh tự miễn khác có thể làm tăng nguy cơ phát triển hoặc làm bệnh MG trở nên trầm trọng hơn.
- Nhiễm trùng, một số loại thuốc, căng thẳng và phẫu thuật là những tác nhân phổ biến có thể làm trầm trọng thêm các triệu chứng của bệnh nhược cơ.
Nói chuyện với một chuyên gia
Về Trợ cấp đồng thanh toánBệnh nhược cơ (MG) là một rối loạn tự miễn dịch mãn tính, đặc trưng bởi sự yếu các cơ chịu trách nhiệm vận động. Đây là một tình trạng tương đối hiếm gặp, với tỷ lệ mắc bệnh khoảng 150 đến 200 trường hợp trên một triệu.
Các yếu tố nguy cơ gây bệnh nhược cơ là gì? Các yếu tố nguy cơ phổ biến của bệnh nhược cơ bao gồm nam giới lớn tuổi, nữ giới trẻ tuổi và một số dấu hiệu di truyền.
Trong hướng dẫn này, chúng ta sẽ đi sâu hơn vào các yếu tố này. Chúng tôi sẽ giải thích những ai có nguy cơ mắc bệnh nhược cơ cao nhất và thảo luận về nguyên nhân gây ra căn bệnh này mà bạn nên biết.
Bệnh nhược cơ là gì?
Bệnh nhược cơ (MG) là một rối loạn tự miễn dịch mãn tính gây yếu cơ. Tình trạng này xảy ra khi sự giao tiếp giữa dây thần kinh và cơ bị suy yếu.
Bệnh nhược cơ có một số triệu chứng, bao gồm:
- Mệt mỏi mãn tính
- Khó khăn khi đi bộ
- Sụp mí mắt (ptosis)
- Khó khăn khi giữ đầu lên
- Biểu cảm khuôn mặt hạn chế
- Nhìn đôi hoặc nhìn mờ (nhìn đôi)
- Yếu ở cổ, cánh tay hoặc chân
- Các vấn đề về nuốt hoặc nhai
- Khó nói (nói nhỏ hoặc nói giọng mũi)
Mặc dù thường không có cách chữa trị, bệnh nhược cơ có một số các lựa chọn điều trị có thể giúp cải thiện các triệu chứng.
Nguyên nhân gây ra bệnh nhược cơ là gì?
Nguyên nhân chính xác gây ra bệnh nhược cơ vẫn chưa được biết rõ. Tuy nhiên, các chuyên gia y tế tin rằng những thay đổi di truyền cụ thể có thể khiến bạn dễ mắc bệnh này hơn.
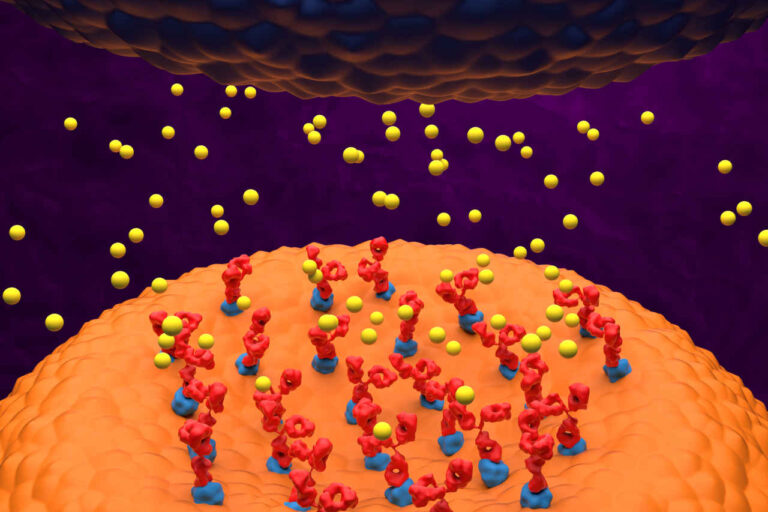
Trong bệnh nhược cơ, hệ miễn dịch sản xuất protein (kháng thể) làm gián đoạn sự giao tiếp giữa dây thần kinh và cơ. Nguyên nhân của hiện tượng này vẫn chưa được hiểu rõ.
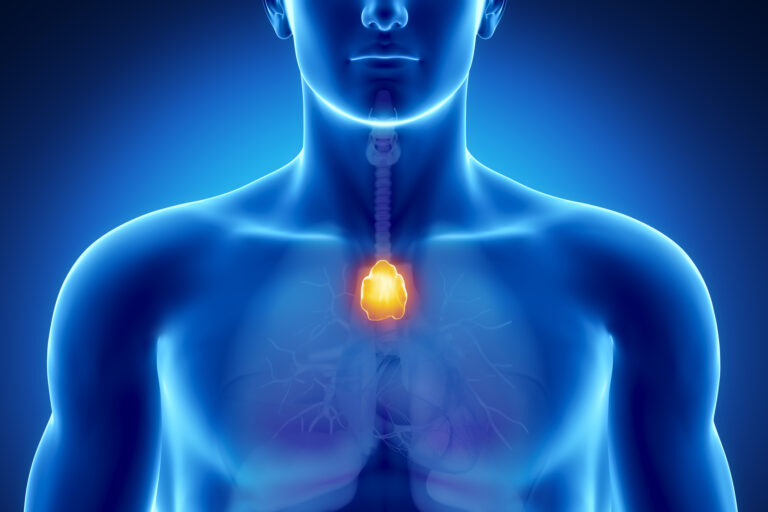
Một số nghiên cứu đã liên kết MG với u tuyến ức (một khối u hiếm gặp hình thành trên tuyến ức). Tuy nhiên, các nhà nghiên cứu vẫn chưa biết ai có nguy cơ mắc bệnh nhược cơ cao nhất và liệu u tuyến ức có phải là nguyên nhân gây bệnh hay không.
Những yếu tố nguy cơ chính gây bệnh nhược cơ là gì?
Các yếu tố nguy cơ chính của bệnh nhược cơ bao gồm:
Tuổi
Bất kỳ ai cũng có thể mắc MG, bất kể tuổi tác. Tuy nhiên, phụ nữ từ 20 đến 39 tuổi và nam giới từ 50 đến 70 tuổi có nhiều khả năng mắc bệnh này hơn [1].
Giới tính
Giống như các bệnh tự miễn khác, bệnh nhược cơ toàn thể ảnh hưởng đến phụ nữ nhiều hơn nam giới. Tỷ lệ nữ/nam mắc bệnh nhược cơ là khoảng 2:1 [2].
Một số phụ nữ có thể gặp các triệu chứng đầu tiên trong thai kỳ. Nhiều phụ nữ cho biết các triệu chứng trở nên nặng hơn trước kỳ kinh nguyệt.
Tuyến giáp

Mắc bệnh tuyến giáp là một yếu tố nguy cơ khác của bệnh nhược cơ, có thể khiến bạn dễ mắc bệnh hơn. Khoảng 5% đến 10% người mắc bệnh nhược cơ có bệnh tuyến giáp [3].
Bệnh tuyến giáp ảnh hưởng đến tuyến giáp ở cổ, nơi sản xuất hormone điều hòa quá trình trao đổi chất. Viêm tuyến giáp Hashimoto, gây suy giáp (tuyến giáp hoạt động kém), và bệnh Graves, gây cường giáp (tuyến giáp hoạt động quá mức), là những bệnh lý phổ biến nhất liên quan đến MG.
Nhận hỗ trợ tài chính
Các bệnh khác
Trong một số ít trường hợp, các rối loạn tự miễn dịch khác có thể làm tăng nguy cơ mắc bệnh nhược cơ. Những người được chẩn đoán mắc các bệnh lý sau đây có thể có nguy cơ mắc bệnh nhược cơ cao nhất:
- Viêm khớp dạng thấp (RA): Viêm khớp dạng thấp là một rối loạn viêm mãn tính ảnh hưởng đến các khớp, gây đau, sưng và cứng khớp. Tuy nhiên, nó cũng có thể ảnh hưởng đến các bộ phận khác, bao gồm da, mắt, phổi, tim và mạch máu.
- Bệnh lupus ban đỏ hệ thống (SLE): Thường được gọi là lupus, SLE là một bệnh tự miễn mãn tính có thể ảnh hưởng đến nhiều bộ phận của cơ thể, bao gồm khớp, da, thận, tế bào máu, não, tim và phổi. Bệnh có thể gây viêm lan rộng và tổn thương mô.
Các yếu tố nguy cơ của bệnh nhược cơ: Giải mã vai trò của di truyền
Người ta cho rằng những thay đổi về gen làm tăng nguy cơ mắc bệnh MG. Tuy nhiên, những gen này vẫn chưa được xác định.
Hơn nữa, MG thường không di truyền và có thể xảy ra ở những người không có tiền sử gia đình. Tiền sử gia đình mắc MG hoặc các bệnh tự miễn khác chỉ xuất hiện ở khoảng 4% các trường hợp [4].
Trẻ sinh ra từ những bà mẹ bị ảnh hưởng hiếm khi bị nhược cơ. Tình trạng này được gọi là nhược cơ nặng ở trẻ sơ sinh. Nhược cơ ở trẻ sơ sinh chỉ là tạm thời. Nếu được điều trị thích hợp, trẻ sẽ hồi phục hoàn toàn trong vòng 60 ngày sau sinh.
Hội chứng nhược cơ bẩm sinh là một nhóm bệnh lý di truyền hiếm gặp tương tự như bệnh nhược cơ nặng nhưng có các yếu tố nguy cơ khác. Bệnh xuất hiện ở trẻ em từ khi sinh ra, với hầu hết các triệu chứng bắt đầu xuất hiện từ thời thơ ấu. Tuy nhiên, trong một số trường hợp, các triệu chứng có thể không xuất hiện cho đến khi trưởng thành. Đây không phải là một bệnh tự miễn và cách điều trị khác với bệnh nhược cơ.
Những yếu tố nguy cơ tiềm ẩn nào khác gây ra bệnh nhược cơ?
Một nghiên cứu năm 2023 cho thấy phụ nữ trên 50 tuổi được chẩn đoán mắc bệnh tiểu đường loại 2 có nguy cơ mắc bệnh nhược cơ cao nhất [5].
Nghiên cứu này đã phân tích dữ liệu từ 118 bệnh nhân MG nhập viện và so sánh họ với một số nhóm đối chứng, bao gồm dân số nói chung và bệnh nhân mắc các bệnh tự miễn khác.
Kết quả nghiên cứu cho thấy phụ nữ trên 50 tuổi mắc bệnh tiểu đường tuýp 2 có nguy cơ mắc MG cao hơn đáng kể. Điều thú vị là bệnh nhân mắc MG do tiểu đường có xu hướng khởi phát bệnh ở độ tuổi lớn hơn so với những người không mắc bệnh tiểu đường.
Nghiên cứu cho thấy bệnh tiểu đường có thể là một trong những yếu tố nguy cơ gây bệnh nhược cơ, đặc biệt là ở phụ nữ lớn tuổi. Tuy nhiên, đây chỉ là những kết quả sơ bộ. Cần nghiên cứu thêm để xác nhận mối liên hệ này và hiểu rõ các cơ chế tiềm ẩn.
Những yếu tố nào có thể khiến bệnh nhược cơ trở nên trầm trọng hơn?
Nếu bạn bị MG, một số yếu tố nhất định có thể làm trầm trọng thêm các triệu chứng hoặc khiến tình trạng bệnh trở nên tồi tệ hơn. Nhận thức được những yếu tố kích hoạt này có thể giúp bạn quản lý sức khỏe tốt hơn và tránh các biến chứng không đáng có. Dưới đây là tổng quan về các yếu tố này.
Sự nhiễm trùng
Nhiễm trùng thường có thể làm trầm trọng thêm các triệu chứng của bệnh nhược cơ. Khi cơ thể chống lại nhiễm trùng, nó sẽ tự nhiên tăng cường phản ứng miễn dịch. Phản ứng tăng cường này có thể làm trầm trọng thêm tình trạng tự miễn dịch tấn công vào khớp thần kinh cơ.
Các bệnh nhiễm trùng thông thường như bệnh đường hô hấp, nhiễm trùng đường tiết niệu hoặc thậm chí cảm lạnh nhẹ có thể dẫn đến tình trạng yếu cơ, mệt mỏi và trong một số trường hợp, có thể dẫn đến cơn nhược cơ.
Điều trị nhiễm trùng kịp thời và duy trì vệ sinh tốt là rất quan trọng để giảm thiểu nguy cơ này. Nếu bạn nhận thấy các triệu chứng trở nặng hơn trong thời gian bị nhiễm trùng, hãy tham khảo ý kiến bác sĩ ngay lập tức.
Nhận hỗ trợ đồng thanh toán ngay
Tiêm chủng
Mặc dù vắc-xin nói chung an toàn và thiết yếu để phòng ngừa các bệnh nghiêm trọng, một số loại vắc-xin có thể đóng vai trò là yếu tố nguy cơ và làm trầm trọng thêm các triệu chứng nhược cơ. Vắc-xin sống hoặc một số loại vắc-xin bổ trợ có thể gây bùng phát bệnh.
Lý do khiến người được tiêm vắc-xin có nguy cơ cao bị các triệu chứng nhược cơ trở nặng hơn là do phản ứng của hệ thống miễn dịch với vắc-xin, có thể làm tăng tạm thời hoạt động tự miễn dịch.
Điều quan trọng là phải thảo luận về tình trạng của bạn với nhà cung cấp dịch vụ chăm sóc sức khỏe trước khi tiêm bất kỳ loại vắc-xin nào. Họ có thể tư vấn về các lựa chọn an toàn nhất, thời điểm tiêm và liệu có cần dùng thuốc dự phòng hay không.
Trong một số trường hợp, việc duy trì lịch tiêm chủng là rất quan trọng để ngăn ngừa các bệnh nhiễm trùng có thể là yếu tố nguy cơ gây bệnh nhược cơ và làm tình trạng bệnh của bệnh nhân trở nên trầm trọng hơn.
Ca phẫu thuật
Các thủ thuật phẫu thuật, đặc biệt là những thủ thuật liên quan đến gây mê hoặc căng thẳng sinh lý đáng kể, có thể ảnh hưởng đến các triệu chứng của MG. Phẫu thuật có thể gây căng thẳng về thể chất và kích hoạt miễn dịch, làm tình trạng yếu cơ tạm thời trở nên trầm trọng hơn.
Một lựa chọn điều trị MG là phẫu thuật cắt bỏ tuyến ức, bao gồm việc cắt bỏ tuyến ức. Tuy nhiên, loại phẫu thuật này đòi hỏi phải lên kế hoạch cẩn thận trước khi phẫu thuật và theo dõi chặt chẽ sau đó.
Thuốc gây mê cũng có thể ảnh hưởng đến sự dẫn truyền thần kinh cơ. Trong những trường hợp này, bác sĩ gây mê có kinh nghiệm về MG phải có mặt trong suốt quá trình phẫu thuật.
Nếu bạn được lên lịch phẫu thuật, điều quan trọng là phải thông báo cho đội ngũ phẫu thuật về chẩn đoán nhược cơ của bạn để họ có thể khắc phục các yếu tố có thể làm trầm trọng thêm tình trạng của bạn. Quản lý tiền phẫu đúng cách có thể giảm thiểu rủi ro và đảm bảo phẫu thuật an toàn hơn.
Một số loại thuốc
Một số loại thuốc điều trị các tình trạng sức khỏe khác có thể ảnh hưởng đến quá trình dẫn truyền thần kinh cơ và làm trầm trọng thêm các triệu chứng MG.
Những loại thuốc nào có thể là yếu tố nguy cơ làm trầm trọng thêm các triệu chứng của bệnh nhược cơ?
- Một số loại thuốc chống sốt rét (ví dụ, quinine và quinidine)
- Thuốc chống co giật (ví dụ, phenytoin, carbamazepine và phenobarbital)
- Một số loại kháng sinh (ví dụ, aminoglycoside như gentamicin và amikacin)
- Thuốc điều trị rối loạn nhịp tim (ví dụ, thuốc chẹn beta như propranolol và metoprolol)
- Statin để hạ cholesterol (ví dụ, atorvastatin, rosuvastatin, simvastatin)
Tốt nhất là tránh những loại thuốc này nếu bạn bị MGTuy nhiên, nếu cần, nên thận trọng khi sử dụng và dùng liều thấp nhất có thể. Thuốc có thể làm suy yếu sự giao tiếp thần kinh-cơ, một yếu tố có thể làm tăng nguy cơ các triệu chứng nhược cơ trở nặng hơn. Hãy hỏi ý kiến bác sĩ để được tư vấn các phương pháp thay thế nếu có thể.
Nhấn mạnh
Người bị căng thẳng về mặt cảm xúc hoặc thể chất cũng có nguy cơ làm trầm trọng thêm các triệu chứng nhược cơ.
Hormone căng thẳng có thể ảnh hưởng đến chức năng miễn dịch và truyền dẫn thần kinh cơ, dẫn đến tình trạng yếu và mệt mỏi. Căng thẳng kéo dài hoặc dữ dội cũng có thể làm giảm ngưỡng chịu đựng của bạn trước cơn nhược cơ.
Phát triển các kỹ thuật quản lý căng thẳng như các bài tập thư giãn, chánh niệm và nghỉ ngơi đầy đủ có thể giúp giảm nguy cơ này. Duy trì thói quen ổn định và tìm kiếm sự hỗ trợ về mặt tinh thần khi cần thiết cũng là những chiến lược hữu ích để kiểm soát các triệu chứng của bạn.
Các yếu tố nguy cơ tái phát bệnh nhược cơ: Những điều bạn nên biết
Trong một số trường hợp, các triệu chứng có thể tái phát ở những người mắc MG đã từng bị cắt bỏ tuyến ức (phẫu thuật cắt bỏ tuyến ức). Nguy cơ cao hơn ở [6]:
- Con đực
- Người lớn tuổi
- Những người mắc bệnh nặng hơn
Nguy cơ tử vong ở bệnh nhân MG có thể cao hơn nếu họ có các triệu chứng nghiêm trọng hơn, đột quỵ, tiểu đường, mức cholesterol cao hơn và nhịp tim bất thường [7].
Nói chuyện với một chuyên gia
Về Trợ cấp đồng thanh toánCác yếu tố nguy cơ của cơn nhược cơ

Cơn nhược cơ (MC) là một biến chứng đe dọa tính mạng của MG. Nó khiến các cơ hô hấp của bạn trở nên quá yếu. Trong những trường hợp nghiêm trọng, bạn có thể cần dùng máy thở.
MC có nhiều khả năng xảy ra nếu bạn có [8]:
- U tuyến ức
- Mức kháng thể cao hơn
- Các triệu chứng nghiêm trọng khi chẩn đoán
Quản lý MG với Nhà thuốc chuyên khoa AmeriPharma®
Hiểu rõ các yếu tố nguy cơ gây bệnh nhược cơ có thể giúp bạn kiểm soát tình trạng bệnh tốt hơn và tránh các biến chứng. Nếu bạn thuộc nhóm có nguy cơ mắc bệnh nhược cơ cao nhất, bạn nên theo dõi chặt chẽ các triệu chứng mới xuất hiện.
Nếu bạn đã được chẩn đoán mắc bệnh MG và cần điều trị, Nhà thuốc Chuyên khoa AmeriPharma® có thể giúp bạn. Nhà thuốc của chúng tôi được chứng nhận ACHC hiệu thuốc chuyên khoa cung cấp các loại thuốc khó tìm cho những người mắc các bệnh lý phức tạp như bệnh nhược cơ.
Liên hệ với chúng tôi hôm nay để nói chuyện với một người hướng dẫn bệnh nhân và bắt đầu nhận điều trị MG với sự phối hợp dịch vụ đầy đủ, hỗ trợ đồng thanh toánvà hỗ trợ 24/7/365.