
La inmunodeficiencia combinada grave (IDCG) es un tipo raro pero grave de trastorno de inmunodeficiencia primaria que aparece en la infancia (a los 6 meses o antes). Los niños que nacen con IDCG tienen un sistema inmunitario muy debilitado. Aunque parecen sanos al nacer, infecciones comunes como la varicela, la neumonía y la meningitis pueden ser mortales debido a un sistema inmunitario gravemente comprometido.
Habla con un especialista
Acerca de la asistencia para copagosEn Estados Unidos, alrededor de 1 de cada 100.000 bebés Cada año nacen niños con IDCG. Anteriormente, muchos niños con IDCG morían en la primera infancia debido a infecciones frecuentes y a la escasez de tratamientos disponibles.
Sin embargo, gracias a los recientes avances científicos, la detección precoz y la intervención temprana en recién nacidos pueden ayudar a tratar con éxito a niños con IDCG.
Analicemos los conceptos básicos del SCID, incluidas sus causas, tipos, síntomas, factores de riesgo, diagnóstico y tratamiento disponible.
¿Qué es la inmunodeficiencia combinada grave?
Inmunodeficiencia combinada grave, también conocida como “niño burbuja o síndrome del niño en la burbuja” es un grupo de trastornos hereditarios (genéticos) que afectan el sistema inmunitario de los recién nacidos. Esta afección se reveló por primera vez tras el estreno de la película para televisión de 1976 sobre David Vetter (una historia centrada en un niño que nació con IDCG y pasó sus 12 años viviendo en una burbuja de plástico para prevenir la infección).
Los niños con IDCG son muy susceptibles a infecciones comunes debido a un sistema inmunitario deficiente. Como resultado, su cuerpo es incapaz de combatir ciertas bacterias, virus y hongos. Esto puede eventualmente provocar una muerte prematura.
¿Qué ocurre en la inmunodeficiencia combinada grave?
Normalmente, el sistema inmunológico de un bebé en desarrollo comienza en la médula ósea, donde las células madre se diferencian en tres tipos diferentes de células: plaquetas, células sanguíneas y glóbulos blancos (GB).
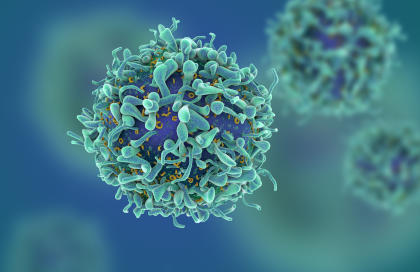
Los glóbulos blancos (GB), en particular, son las células que ayudan al cuerpo a combatir ciertos patógenos (p. ej., bacterias, hongos y virus) para prevenir infecciones o enfermedades. Existen varios tipos de GB, incluyendo los linfocitos, que son células B y células T que realizan las siguientes funciones:
- células T Identificar, atacar y matar el patógeno.
- células B funcionan como células de memoria (células que recuerdan o memorizan el patógeno causante de la infección) y células plasmáticas (células que producen anticuerpos en caso de que el cuerpo se exponga nuevamente al patógeno).
En los niños con IDCG, ambos linfocitos (células T y B) están afectados o prácticamente ausentes. Como resultado, el sistema inmunitario se debilita considerablemente y no funciona correctamente para combatir los patógenos causantes de infecciones.
¿Qué causa la inmunodeficiencia combinada grave (SCID)?
La SCID se produce debido a mutaciones genéticas en múltiples genes de los cromosomas X. Estos genes participan principalmente en el desarrollo y el funcionamiento de las células inmunes, como las células B, las células T y las células asesinas naturales (células NK).
La IDCG es un trastorno recesivo ligado al cromosoma X y solo afecta a los hombres, ya que solo tienen un cromosoma X. Las mujeres pueden ser portadoras y transmitir los genes defectuosos a sus hijos varones. Sin embargo, en más de... 80% de casosLos niños con SCID no muestran antecedentes familiares de SCID.
¿Cómo se clasifica la inmunodeficiencia combinada grave (SCID)?
Los proveedores de atención médica han clasificado la IDCG en varios tipos según el tipo de defectos genéticos. En 15% de casosSe conocen defectos genéticos. A continuación, se presentan algunos tipos de IDCG:
SCID clásica ligada al cromosoma X
La SCID clásica ligada al cromosoma X se produce como resultado de una mutación en un gen (Gen IL2RG) ubicado en el cromosoma X. En este tipo, los glóbulos blancos crecen y se desarrollan de forma anormal. Como resultado, los pacientes con esta afección presentan un recuento bajo de linfocitos T, linfocitos B y linfocitos citolíticos naturales (NK) que no funcionan. Este tipo afecta principalmente a los varones, ya que solo tienen una copia del cromosoma X.
SCID por deficiencia de ADA
En este tipo, una mutación en el gen ADA provoca una deficiencia de la enzima ADA, necesaria para la supervivencia de las células T. Los médicos llaman a este tipo SCID por deficiencia de ADA.
SCID con fugas
En este tipo, el niño tiene células T notables o incluso en exceso, que causan inflamación y daños al cuerpo.
Obtenga autorización previa para IgIV
Cómo identificar si su hijo tiene inmunodeficiencia combinada grave (IDCG)
Los signos y síntomas de la IDCG suelen aparecer entre los 3 y los 6 meses de edad y generalmente incluyen infecciones respiratorias frecuentes, candidiasis común, diarrea crónica y neumonía fúngica. Otros síntomas notables pueden incluir:
- Erupciones
- Infecciones de oído
- Crecimiento lento
- Problemas para ganar peso
- Infecciones que no responden bien a los antibióticos
- Candidiasis recurrente (infección por hongos) en la boca
Si su hijo presenta los síntomas mencionados anteriormente, especialmente neumonía fúngica, consulte de inmediato a su proveedor de atención médica para que le realice pruebas genéticas y detección de SCID.
¿Cuál es el procedimiento de diagnóstico de la inmunodeficiencia combinada grave (SCID)?
El diagnóstico y la detección precoces de la IDCG pueden aumentar la tasa de éxito en la lucha contra esta enfermedad. Un profesional de la salud realiza una prueba de sangre mediante punción en el talón para verificar el nivel de células T y anticuerpos en el organismo del niño.
Dependiendo de los resultados de los análisis de sangre, se pueden realizar más pruebas para comprobar los marcadores genéticos de SCID mediante pruebas genéticas.
¿Cómo se trata la SCID?
La IDCG es una afección grave que requiere tratamiento pediátrico de emergencia inmediato. Sin tratamiento, los niños con IDCG no sobreviven más allá del primer año de vida. Sin embargo, el tratamiento temprano puede mejorar significativamente el pronóstico. A continuación, se presentan algunas de las opciones de tratamiento disponibles actualmente para la IDCG:
Trasplante de médula ósea
El trasplante de médula ósea es un tratamiento estándar y eficaz para bebés con IDCG. En este procedimiento, se trasplantan células madre hematopoyéticas (también conocidas como hematopoyéticas) de la médula ósea de donantes compatibles a pacientes con IDCG. Esto reconstituye el sistema inmunitario de los pacientes con IDCG y les permite desarrollar un sistema inmunitario funcional.
El donante para trasplantes de médula ósea podría ser un familiar cercano, como hermanos sanos o padres. Sin embargo, en la mayoría de los casos, los pacientes no tienen donantes hermanos compatibles, por lo que a menudo se realizan trasplantes de donantes compatibles no emparentados, lo que tiene una tasa de éxito menor que la de un donante emparentado compatible.
Además, el trasplante temprano de médula ósea suele ofrecer los mejores resultados para los bebés con IDCG. Por ejemplo, los investigadores examinaron datos de 240 bebés con IDCG y descubrieron que, independientemente del tipo de donante de células madre, Los bebés que recibieron trasplantes antes de los 3,5 meses de edad tuvieron la mayor probabilidad de supervivencia.
Terapia de reemplazo enzimático
La terapia de reemplazo enzimático (TRE), como la PEG-ADA, es una opción de tratamiento para bebés con inmunodeficiencia combinada grave (IDCG) por deficiencia de ADA. En esta terapia, se inyecta regularmente un medicamento para tratar la deficiencia de ADA. Esta terapia ayuda a prevenir infecciones frecuentes, restaurar la función inmunitaria y, indirectamente, favorece el crecimiento infantil al promover una mejor salud general.
Sin embargo, la TRE es sólo una opción de tratamiento temporal y se utiliza hasta que el paciente encuentre un donante de células madre para el trasplante.
Terapia génica
Terapia genética Puede ser un tratamiento eficaz para algunos SCID ligados al cromosoma X. También es una opción para los bebés con SCID que no son elegibles para trasplantes de células madre o no pueden encontrar el donante adecuado.
En este procedimiento, el profesional de la salud obtiene las células madre del niño con IDCG y reemplaza el gen defectuoso por uno normal en el laboratorio. Posteriormente, las células madre con el nuevo gen sano se insertan nuevamente en la médula ósea del niño con IDCG.
La terapia genética es experimental y todavía se encuentra en la fase de ensayos clínicos en EE. UU.
Inmunoglobulina intravenosa (IVIG)
IgIV La terapia es otra opción de tratamiento eficaz para bebés con IDCG para controlar las posibilidades de infecciones recurrentes. La IgIV proporciona una amplia gama de anticuerpos para pacientes con SCID que refuerzan el sistema inmunológico y ayudan a sus cuerpos a combatir infecciones.
Consulte a un especialista en IgIV
Llevar
La IDCG es un trastorno genético poco común pero grave que puede ser mortal, incluso con infecciones comunes, si no se diagnostica y trata durante el primer año de vida. La terapia génica, la inmunoglobulina intravenosa (IVIG), la terapia de reemplazo enzimático y los trasplantes de médula ósea son tratamientos disponibles para ayudar a su hijo a llevar una vida saludable. Consulte con su profesional de la salud si desea realizarle pruebas genéticas o si tiene alguna inquietud sobre la salud de su hijo.
REFERENCIAS:
- PATEL, AC, y REN, CL (2004). Complicaciones pulmonares de los trastornos inmunológicos. Neumología pediátrica, 140-150. https://doi.org/10.1016/B978-0-323-01909-5.50016-5
- Donda, K., Torres, BA, Walter, J., y Maheshwari, A. (2023). Síndromes de inmunodeficiencia observados durante el período neonatal. Principios de neonatología, 498-506. https://doi.org/10.1016/B978-0-323-69415-5.00057-6
- Vaillant, A. a. J., y Mohseni, M. (2023). Inmunodeficiencia combinada grave. StatPearls - Estantería NCBI. https://www.ncbi.nlm.nih.gov/books/NBK539762/
- Inmunodeficiencia combinada grave (IDCG). (2019). NIA]ID: Instituto Nacional de Alergias y Enfermedades Infecciosas. https://www.niaid.nih.gov/diseases-conditions/severe-combined-immunodeficiency-scid#:~:text=Severecombinedimmunodeficiency(SCID)is,highlysusceptibletosevereinfections
- Nhgri. (2019). Acerca de la inmunodeficiencia combinada graveGenome.gov. https://www.genome.gov/Genetic-Disorders/Severe-Combined-Immunodeficiency
- Agarwal, S., y Cunningham-Rundles, C. (2019). Manifestaciones y complicaciones gastrointestinales de los trastornos de inmunodeficiencia primaria. Clínicas de Inmunología y Alergia de América del Norte, 39(1), 81-94. https://doi.org/10.1016/j.iac.2018.08.006
- Winkelstein, JA (2006). Enfermedades de inmunodeficiencia primaria. Medicina Hospitalaria Pediátrica Integral, 864-869. https://doi.org/10.1016/B978-032303004-5.50140-X
- Cirillo, E., Giardino, G., Gallo, V., Grasso, F., Romano, R., Lillo, CD, Galasso, G. y Pignata, C. (2015). Inmunodeficiencia combinada grave: una actualización. Anales de la Academia de Ciencias de Nueva York, 1356(1), 90-106. https://doi.org/10.1111/nyas.12849













