Nutrition is important in many aspects of health, including immune function, growth, and healing. Certain diseases can hinder the body’s capacity to effectively absorb or utilize essential nutrients, while other ailments can disrupt a person’s ability to eat or result in reduced appetite.
Always in Stock
Full inventory of IV fluids, ready for youIntervention may be warranted to augment nutritional support and mitigate the deterioration of health during times of sickness. Medical professionals have two viable options at their disposal for delivering essential calories, vitamins, electrolytes, and minerals: enteral and parenteral nutrition, each offering distinct avenues for nourishing the body. The main difference between enteral vs. parenteral nutrition is the route of administration.
Enteral nutrition is the administration of nutrients via the gastrointestinal tract, whereas parenteral nutrition is the administration of nutrients via alternative routes, such as intravenously via a catheter. While specific formulations depend on health problems, activity level, and caloric requirements, this guide will provide an overview of each supplemental nutrition regimen and discuss their differences.
Enteral and Parenteral Nutrition Delivery
Typically, a team of physicians, dieticians, and pharmacists determine whether someone needs a supplemental nutrition program. Before any nutrients can be provided, an appropriate means of delivery for enteral vs. parenteral nutrition must be established.
Enteral Nutrition Delivery
Enteral nutrition, which involves feeding nutrients directly into the stomach, can be accomplished with a tube inserted through the nose or mouth and passed down the esophagus. This method is commonly used for individuals who are at risk of choking on oral feeds or are unable to self-feed for an extended period of time.
Medical conditions can sometimes prevent the stomach from emptying properly. A tube may be advanced in these cases to deliver nutrients past the stomach and directly into the small intestine.
A percutaneous endoscopic gastrostomy (PEG) tube may be implanted via surgery. The PEG tube provides a direct path through the abdomen to the stomach. While this involves surgery, it is generally the best long-term option when considering enteral vs. parenteral nutrition, as it is better tolerated and has fewer risks than a tube in the esophagus or veins.
Parenteral Nutrition Delivery
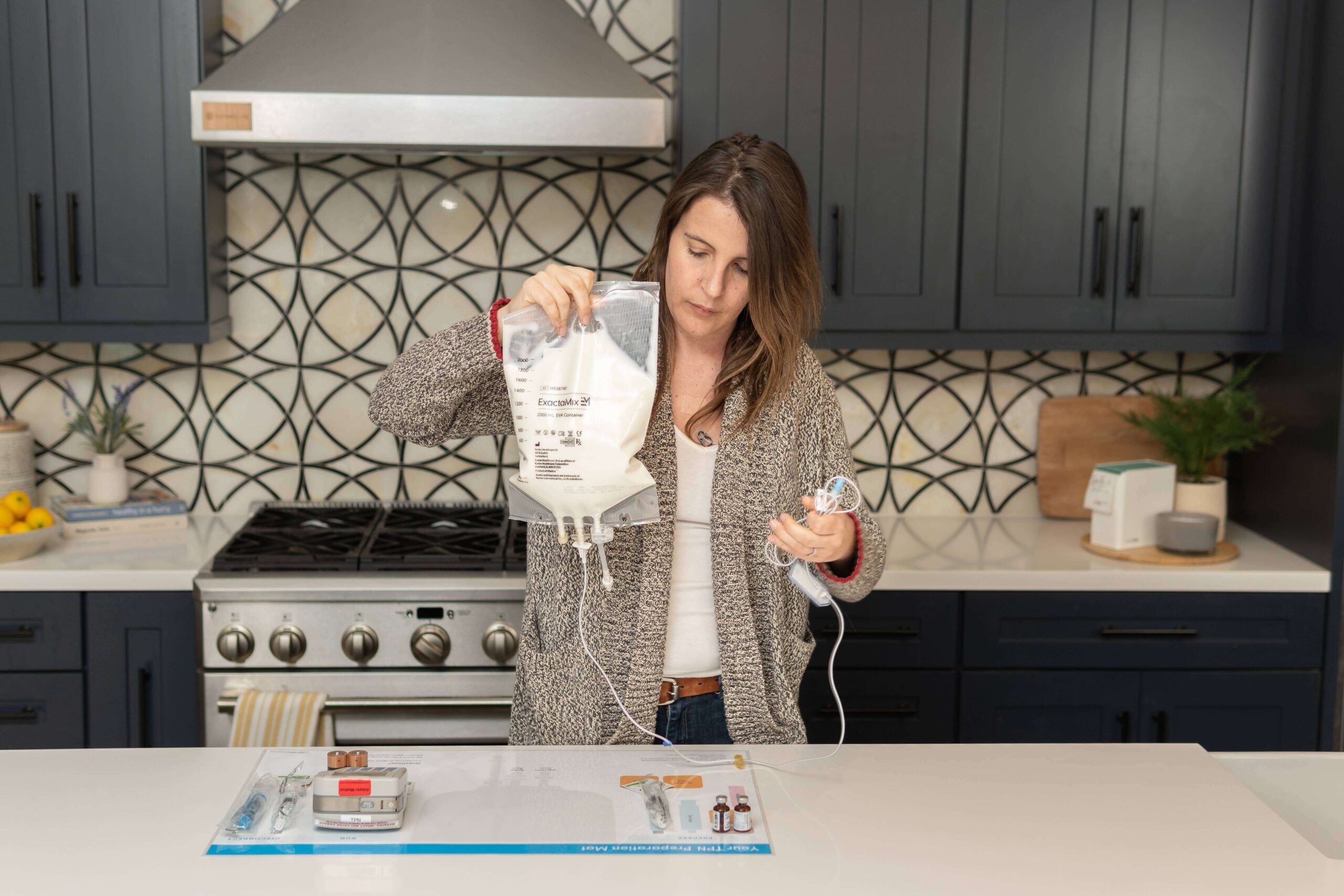
Total parenteral nutrition (TPN) is when all nutrients are administered through a central vein, completely bypassing the intestinal system. TPN is usually administered via an IV catheter, although the location may vary. If parenteral nutrition is to be administered for several days, the catheter is inserted in a large, central vein, such as the jugular vein in the neck.
Peripheral parenteral nutrition (PPN) makes use of the small, peripheral veins in the extremities. These veins cannot handle the large load and highly concentrated formulation of parenteral nutrition for extended periods. The IV catheter in PPN must be replaced somewhat frequently, given the irritation it can cause to veins.
An implanted port may be surgically inserted under the skin for more long-term parenteral nutrition delivery. To administer the nutrients, a needle can be inserted into this port, which is attached to a sizable vein. The port is simpler to use and, in the long run, reduces the frequency of needle sticks.
Composition of Enteral vs. Parenteral Nutrition
The nutritional needs of each individual determine the feed’s composition. People with kidney failure, for instance, may need special formulations because they may have trouble excreting electrolytes and fluids from the body. However, all necessary nutrients, such as carbohydrates, amino acids, electrolytes, vitamins, and fats, can be given in both enteral and parenteral nutrition programs.
There are numerous formulations for enteral programs, each with a unique caloric density and composition. The majority of people can usually get by with the enteral nutrition standard formulation. It contains roughly 1 kcal/L in a mixture of protein, fats, carbohydrates, vitamins, and minerals and has the same concentration as blood.
As the name implies, concentrated formulations for enteral vs. parenteral nutrition contain less fluid and are frequently used by people who need to limit their fluid intake. Some enteral formulations may contain predigested nutrients (e.g. short-chain peptides and simple carbohydrates) with lower fat content to make it easier to absorb.
Amount and Rate of Feeds in Enteral and Parenteral Nutrition Programs
Feeds can be scheduled to be run continuously or as a bolus. The majority of feeds are given continuously, though one may not always be superior to the other. Whether it is enteral vs. parenteral nutrition, a multidisciplinary team decides on the necessary amount based on the individual needs of each person.
There are two methods for starting the feeding schedule for enteral nutrition. The medical staff may opt to begin more slowly and build up to the desired rate. The recipient may tolerate this route better, which may result in fewer side effects like vomiting or constipation. The alternative strategy entails starting the feeds right away at the desired rate.
Usually, parenteral nutrition is given continuously for 24 hours. If the patient can tolerate it, the infusion can be adjusted to last for a shorter time. This makes it more convenient for people adjusting to life with parenteral nutrition at home.
AmeriPharma® Specialty Care
Total Parenteral Nutrition | Leader In TPN AssistanceComplications of Enteral vs. Parenteral Nutrition

As with any medical intervention, enteral and parenteral nutrition programs may have some complications. It is crucial to be aware of these potential problems so that they can be quickly resolved.
Enteral Complications
During enteral feeding, aspiration may obstruct the airway or result in secondary complications like pneumonia. There are numerous tactics that can be used to lower the risk of aspiration. These include feedings while standing up or delivering food past the stomach (e.g. nasojejunal tube or PEG tube). Additionally, drugs that speed up stomach emptying can lessen the chance of motion sickness and aspiration.
It is important to highlight that enteral feeds typically lack the adequate amount of water to fulfill the recommended daily amount. Nevertheless, the feeding tubes are routinely flushed with water to prevent clogging, which may suffice to meet the desired water intake goals. Additional side effects that are unique to enteral feeds vs. parenteral nutrition are diarrhea or constipation.
Parenteral Complications
The risk of infection is slightly increased because parenteral nutrition is given directly into the bloodstream. This risk can be minimized through proper technique when administering TPN and good individual hygiene overall.
Further, as venous access is required for parenteral nutrition, there is a risk of vascular injury, which can lead to complications with TPN, such as bleeding and blood clots. Rarely, more severe complications such as pneumothorax or air embolus can develop.
The motility of the gallbladder and digestive tract is reduced as a result of parenteral nutrition bypassing the intestines. This could result in an accumulation of bile in the liver and gallbladder, which could irritate these organs and cause widespread itching as bile acids enter the bloodstream.
Complications with Enteral and Parenteral Nutrition
There are a few potential side effects that may be seen in either enteral vs. parenteral nutrition. Hyperglycemia and electrolyte imbalances are the most common complications. These abnormalities are typically mild and treatable quickly.
The sudden surge of electrolytes and fluids in chronically malnourished individuals can cause refeeding syndrome, in which large amounts of insulin are released, causing phosphate, potassium, and magnesium to enter cells. These electrolyte imbalances can cause additional complications. As a result, for malnourished people, sudden increases in calories are avoided, and initial feeds are closely monitored by medical professionals.
Get Financial Assistance for TPN
Monitoring in Enteral vs. Parenteral Nutrition
People who receive supplemental nutrition may benefit from monitoring in the early stages. This is especially true if they have a complicated medical history. Fluid restriction, for example, may be required for certain medical conditions such as kidney disease or heart failure. In such cases, an accurate log of intake and output can be kept.
Electrolyte levels should be monitored in the first few weeks, especially for malnourished patients who are at a higher risk of refeeding syndrome. Enzymes, triglycerides, vitamins, and minerals may also be measured on a weekly or monthly basis to address imbalances. Once the intervals between measurements are stable, they can be spaced out.
Receive TPN at Home with AmeriPharma® Specialty
AmeriPharma® Specialty Pharmacy is a full-service, triple-accredited pharmacy dedicated to assisting people with complex medical conditions receive necessary treatments. We will advocate to get insurance approvals and work to obtain 공제금 지원 to reduce your treatment costs. We strive to make getting treatment as easy as possible. This is why we provide discreet prescription deliveries to homes in over 40 states.
We specialize in hard-to-access treatments, including IVIG, parenteral nutrition, and chemotherapy. With over 20 years of expertise, we streamline the treatment process to make your life simpler. We offer home infusion services with specialized nurses who will also teach you how to best manage your care. Explore our blog to learn more about enteral vs. parenteral nutrition and other specialty medical treatments.
Contact AmeriPharma® Speciality at (877) 778-0318 for more helpful information or to speak with one of our experts about your treatment options. Our dedicated staff is available 24 hours a day, seven days a week to answer questions and provide dependable care tailored to your specific needs. Consult AmeriPharma® Speciality for expert care that is safe, dependable, and effective.













